Knock Knees
What are knock knees?
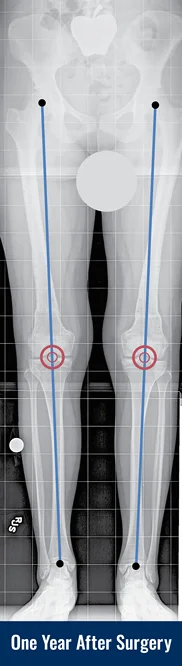
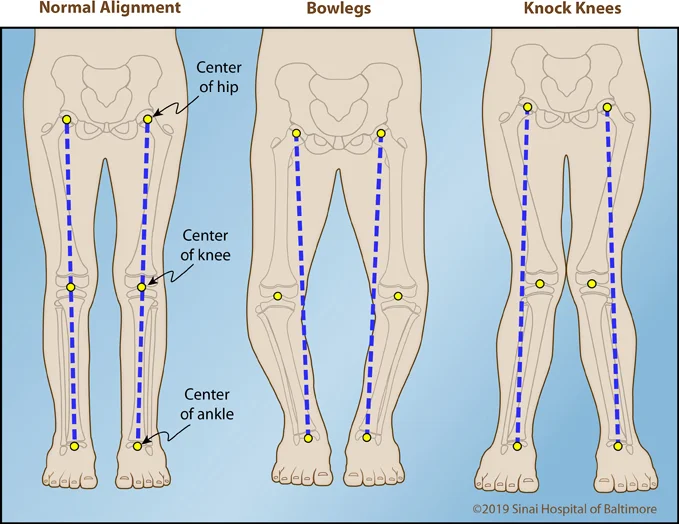
Knock knees are legs that curve inward at the knee, often preventing the ankles from coming together without shifting one knee in front of the other. In order to understand knock knees, also called genu valgum, it is important to first understand “normal” alignment of the legs. In the normal situation, when standing, the hips, knees and ankles all fall on a straight line. In other words, when you draw a line from the hip to the ankle, that line passes directly through the center of the knee. If that line passes to the outside of the knee (externally), this is called knock knees (valgus deformity). If that line passes to the inside of the knee (internally), this is called bowlegs (varus deformity).
The International Center for Limb Lengthening has taken care of many adults and children with knock knees. Many toddlers have knock knees that will correct on their own during their elementary school years; if they do not, surgical correction may be deemed necessary. In adults, knock knees do not resolve spontaneously, but rather tend to worsen as arthritis leads to further malalignment. Knock knees in adults are an independent risk factor for knee joint degeneration and pain. It has been demonstrated that correction of knock knees prior to the onset of end stage arthritis can delay or prevent the need for total knee replacement.
What causes knock knees in children?
Knock knees in children can be caused by:
- Normal developmental knock knees with peak incidence at age three to four years
- Idiopathic (no known cause), usually appears in adolescence
- Renal rickets (associated with kidney failure and renal osteodystrophy—a bone disease that occurs when your kidneys fail to maintain proper levels of calcium and phosphorus in the blood)
- Nutritional rickets and vitamin D-deficiency
- Hypophosphatemic rickets (vitamin D-resistant rickets)
What causes knock knees in adults?
In adults, knock knees can be caused by trauma or infection, arthritis or residual effects from pediatric orthopedic disease.
How is knock knees diagnosed?
On physical appearance, with the patient standing upright, the knees touch each other, but there is a wide space between the ankles. The best way to diagnose knock knees is by taking a standing X-ray, and drawing the straight line on the image from the hip to the ankle. If that line passes to the outside of the knee, there is genu valgum present. Additional diagnostic lines can be drawn to determine if the source of the angular deviation is coming from the femur (thigh bone) or the tibia (shin bone).
When looking at children’s X-rays, we also pay attention to the quality of the bone and the width of the growth plates. (Growth plates are responsible for children’s arms and legs getting longer as they mature.) Children with nutritional vitamin D deficiency, vitamin D-resistant rickets (disorder in which the bones become painfully soft and bend easily), or with kidney failure, for example, have widened, irregular growth plates and can present with genu valgum. In children where vitamin D deficiency, vitamin D-resistant rickets, or kidney failure are suspected as the cause of knock knees, additional blood tests (i.e., complete blood count, phosphorus, vitamin D level, creatinine, calcium) can be done to specifically look for those issues.
What is the recommended treatment for knock knees?
The aim of treatment will be to correct limb alignment, stop disease progression, and reduce the risk of joint degeneration. Many children will present with knock knees in their toddler years. This can be a normal tendency in children and typically does not require any treatment. However, if X-rays look abnormal (i.e, excessively wide or irregular growth plates) or the child looks pale and sickly, then further work up (i.e., blood tests) is needed. If there are abnormalities of metabolism or kidney function, then special medical treatment is needed. For example, nutritional rickets is treated with vitamin D replacement. Vitamin D-resistant rickets (X-linked hypophosphatemic rickets) is treated with vitamin D and phosphorous replacements, and more recently, the drug Berosumab (Crysvita). If medical treatment is not successful in getting the legs to straighten, then surgery may be required. In idiopathic cases (where the cause is unknown), treatment can be done surgically.
In growing children, it is possible to do very small, minimally invasive surgeries that will modulate the growth of the legs, getting them to grow straight over a period of 6-18 months. This is done by implanting a staple or plate with screws next to the growth plate, on the convex side of the limb deformity (i.e., the inner knee for genu valgum). These treatments generally don’t require limited weight bearing or much physical therapy. For more information on this treatment, please see Guided Growth (Hemiepiphysiodesis).
In adults and older children with less than two years of growth remaining until maturity, this guided growth treatment is not an option. Instead, we must cut the affected bones (osteotomy) and straighten them in one of two ways:
- Acute osteotomy:
The bone is cut and full correction is done in the operating room. The patient will typically have a plate with screws inserted internally to stabilize the cut bones and will be non-weightbearing for a period of 6 to 8 weeks until the bone unites.
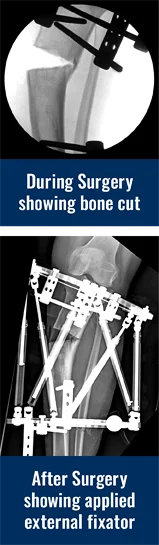
- Gradual correction using an external fixator (see images of Georgina above):
The knock knee leg can be corrected gradually using an adjustable frame. The surgeon cuts the bone, and applies an adjustable external frame that is connected to the bone with wires and pins. The parents receive a regimen outlining the daily adjustments that should be done to the frame. The patient walks, sleeps, bathes and does all his or her daily activities with the frame in place. The bone gradually heals in the corrected position, and the patient visits the doctor every few weeks to make sure that everything is going as planned. Based on follow up X-rays, the doctor may revise the schedule in order to achieve better results. After correction, the frame will need to be removed in the operating room.
Which treatment plan is best for me?
The treatment plan is decided based on many factors:
- bone maturity,
- the nature of the disease and its tendency to progression,
- the severity of that disease,
- the presence of shortening requiring lengthening,
- an abnormality or depression in the knee joint line, and
- patient/family preference.
All of these factors will dictate the surgeon’s recommendation.
Why choose the International Center for Limb Lengthening for knock knee treatment?
The International Center for Limb Lengthening is world-renowned for its expertise in limb deformity correction. Your doctor will take the time to make sure you understand all of your options and then will customize your treatment to meet your specific needs. Our patients benefit from our team-centered approach with world-renowned pediatric and adult orthopedic surgeons and specialized physician assistants, nurses and physical therapists. We help patients with knock knee achieve their best possible result.