Congenital Pseudarthrosis of the Tibia
What is congenital pseudarthrosis of the tibia?
Congenital pseudarthrosis of the tibia (CPT) is a shin bone fracture in children that has not healed. It normally presents before a child turns two years old. Typically, the child gets a shin bone fracture that either happens spontaneously, or results from when the child experiences a minor trauma, and the fracture does not heal. It is a rare condition that occurs in 1 out of every 250,000 children.
It stems from the periosteum, a membrane that covers the bone, being abnormal and preventing proper bone healing. Since the bone has not healed correctly, it is unstable and there is mobility at the false joint which should be solid, stable bone. As a result, many patients have an unstable leg, making function difficult.
 CJ (#14) playing lacrosse after successful CPT treatment. For more of CJ’s story, click here.
CJ (#14) playing lacrosse after successful CPT treatment. For more of CJ’s story, click here.Historically, congenital pseudarthrosis of the tibia was known as an extremely challenging problem to treat, because it was very difficult to get the fractured bone to heal with techniques that were available in the past. Advances in medical treatment as well as surgical techniques have generated vast improvements in outcome. While refracture is a potential risk, current treatment protocols have minimized this formerly devastating complication.
Basic science and surgical research have shown that the poor healing is due to the irregular periosteum, abnormally hyperactive osteoclasts (cells that remodel bone), and the mechanical challenge of stabilizing very small bone fragments in children. A multifaceted approach addresses each component of the problem individually.
A secondary effect of CPT is limb length discrepancy, which must be factored in to the overall treatment plan to ensure an optimal reconstructive outcome.
Video: Congenital Pseudarthrosis of the Tibia: CJ’s Story
Who gets congenital pseudarthrosis of the tibia?
Many children with congenital pseudarthrosis of the tibia are also diagnosed with neurofibromatosis (NF-1), a genetic condition which has many other serious potential manifestations. However, congenital pseudarthrosis of the tibia is also seen in fibrous dysplasia, osteofibrous dysplasia and cleidocranial dysostosis. The exact cause of CPT is unknown (“idiopathic”).
How is congenital pseudarthrosis of the tibia diagnosed?
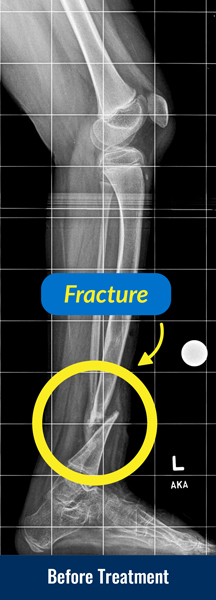
Congenital pseudarthrosis of the tibia is typically identified with X-rays and physical examination. Patients who are deemed high risk (e.g., patients with neurofibromatosis) may have screening X-rays performed in early childhood. In some cases, the first sign is a deformity in the leg or a fracture that occurred with minimal trauma.
What will happen during a clinic visit for congenital pseudarthrosis of the tibia?
The doctor will evaluate the patient for neurofibromatosis which may be diagnosed with genetic blood testing. The doctor will also ask for a history of previous fractures and examine the leg to determine the range of motion of the false joint. X-rays will be taken to determine the quality of the bone, the condition of the joints, the amount of limb length discrepancy and the severity of any bone abnormalities.
How is congenital pseudarthrosis of the tibia treated?
The primary treatment goal of congenital pseudarthrosis of the tibia is to achieve union of the shin bone (tibia) and to maintain that union. Treatment also addresses the resulting limb length discrepancies and bone deformities. To treat congenital pseudarthrosis of the tibia, the International Center for Limb Lengthening has a combined multimodal, comprehensive cross-union treatment program that addresses both the biological and mechanical issues. Many doctors use various elements of our protocol, but we strongly believe that the combined multimodal cross-union approach is the most effective.
What happens in cross-union surgery for congenital pseudarthrosis of the tibia?
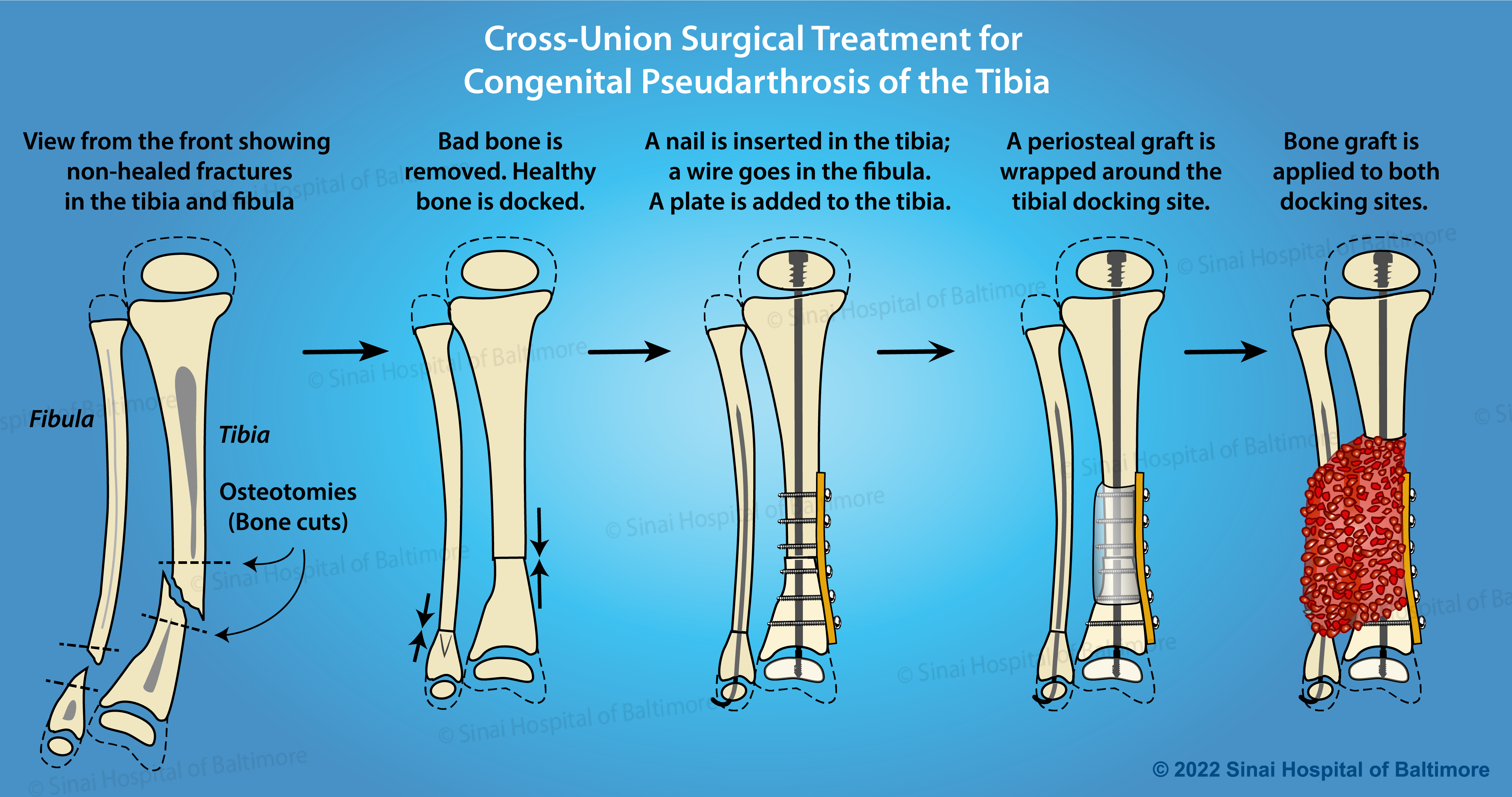
Cross-Union Surgery for Congenital Pseudarthrosis of the Tibia Treatment Steps
- Two to four weeks before surgery, the patient receives a bisphosphonate infusion from our endocrinologist. Bisphosphonates inhibit cells responsible for breaking down bone. It is used to prevent resorption (melting away) of bone graft and to improve local healing response. This can take place in Baltimore, or for patients from further away, it can be done closer to home by a local endocrinologist.
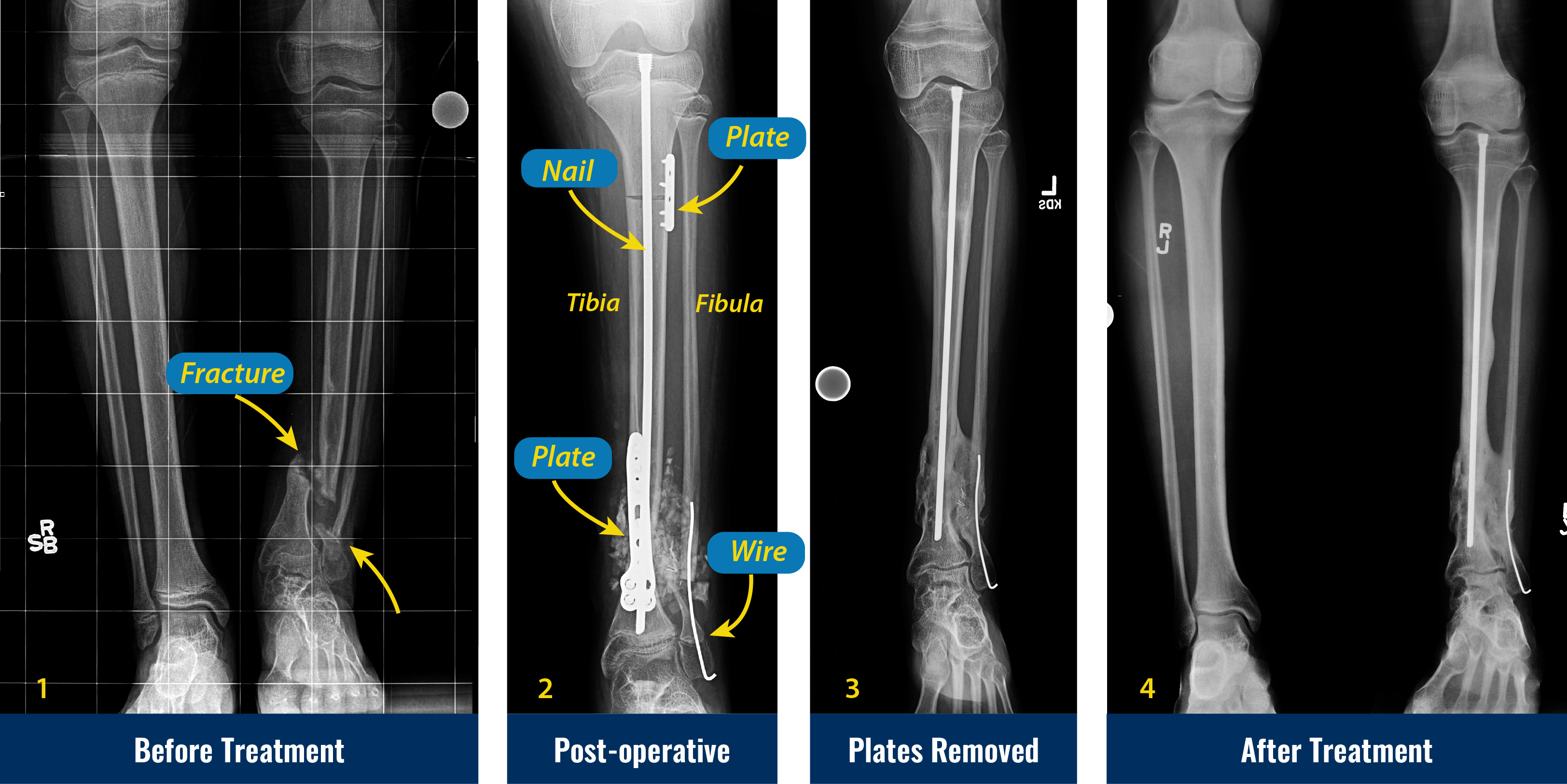
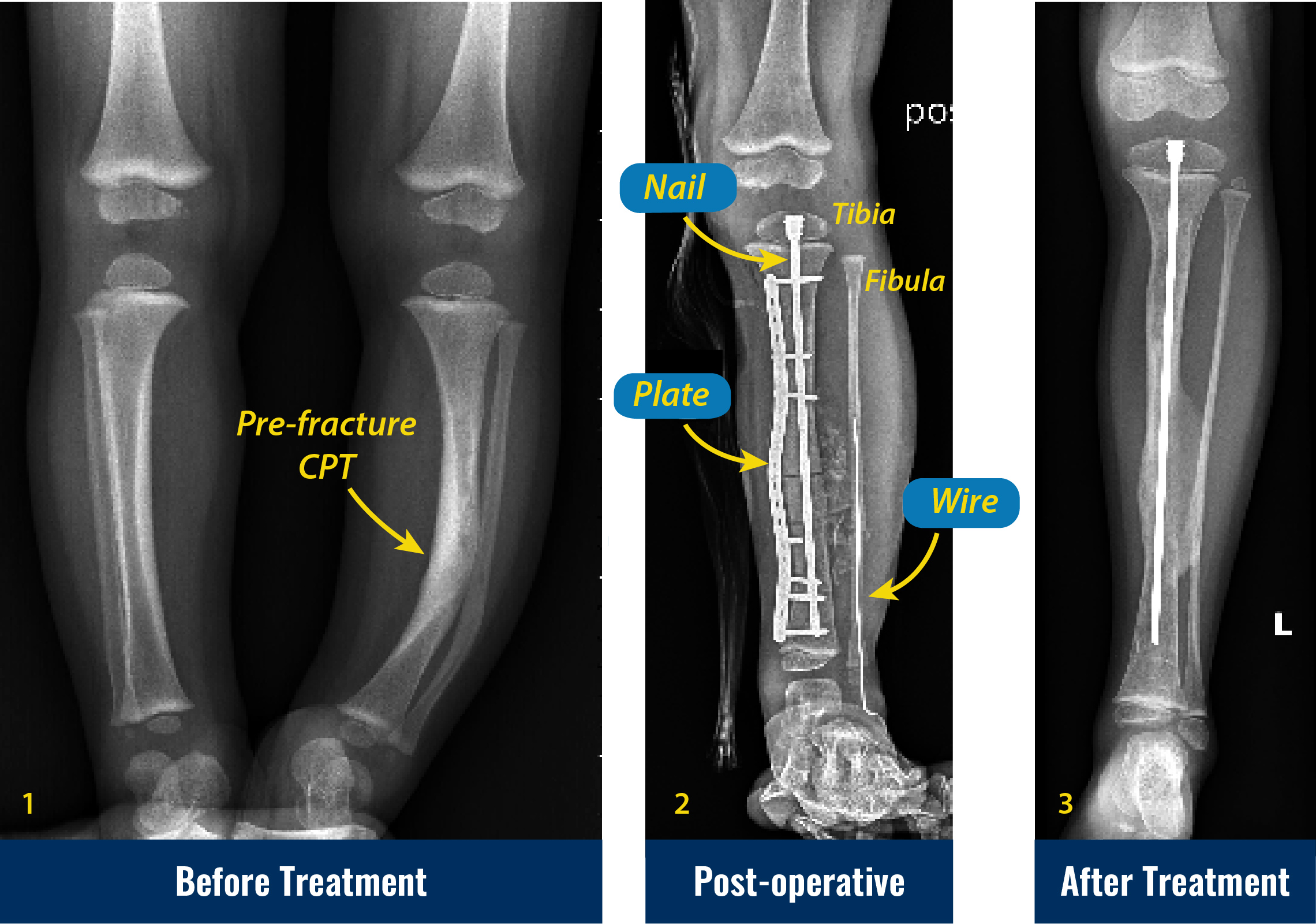
- In the operating room, the abnormal periosteum is removed from the tibia and fibula (both bones in the lower leg), and the pencil tip ends of the tibia and fibula are slightly trimmed to allow straightening of the leg with stable bone contact to optimize healing.
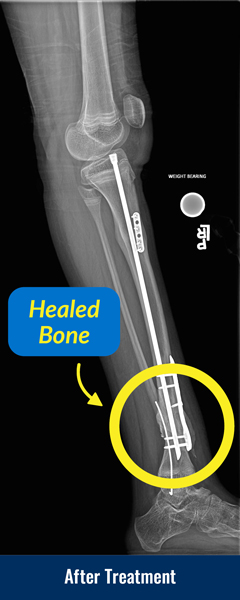
- The tibia is stabilized with intramedullary rods (placed inside the canal of the bone), and the fibula is stabilized with wires. Newer intramedullary rods have allowed surgeons to avoid crossing and damaging the ankle joint.
- Healthy periosteum and a bone graft are harvested from the pelvis usually on the same side as the tibia pseudarthrosis.
- The healthy periosteum, bone graft, and bone morphogenic protein (BMP) are placed in between and around the tibia and fibula bones, generating a large cross-sectional surface area for optimal healing. BMP is a naturally occurring cell signaling molecule that drives bone formation. When used in CPT treatment, it helps increase bone formation in the early stages. While healing can occur without BMP, it is an important component of the International Center for Limb Lengthening’s multi-faceted approach.
- In most cases, an internal modern locking plate is used to control the newly realigned limb. In the past, an external fixator was applied to the leg to provide rotational stability and to compress the bone ends while they healed. The combination of newer ankle-sparing intramedullary rods and improved internal plates gives surgeons another option to maintain improved ankle motion.
- Once healing has occurred (typically evident by 2 months, and strong by 3-4 months), activity restrictions are lifted, and children can return to normal activities. A plastic leg brace called an ankle foot orthosis (AFO) is worn on the leg under clothing for additional protection.
- The plate is removed 6-12 months after the initial surgery, while the rods remain inside to act as “rebar” to strengthen the newly healed leg and prevent refracture.
- Regular monitoring of the bone is required on an annual basis. The internal rod may need to be swapped out every 3-4 years during childhood as the leg grows longer to keep providing protection against refracture.
What happens after congenital pseudarthrosis of the tibia surgery?
After the cross-union surgery, patients return monthly to clinic for follow-up visits until the bone heals. Three to four months after surgery, another infusion of bisphosphonate is done to prevent the bone graft from resorbing. After the bone has healed, patients return annually for checkups. We have seen very successful results with this combined cross-union treatment at all ages. After skeletal maturity, the bone becomes more normal and does not have as much tendency to fracture again.
Additional surgery may be needed in the future for limb lengthening or to insert longer rods to accommodate growth. Ankle deviations are common and may require realignment surgery. While our success rate with the multimodal approach is very high, nothing is 100%. We have found that some children require a second surgery to achieve union or to treat a refracture. Thanks to advances at our center and around the world, the risk of refracture is minimal.
What is the “unbroken” congenital pseudarthrosis of the tibia?
Some children with congenital pseudarthrosis of the tibia are born with the leg crooked, but not broken. In such cases, we recommend bracing to prevent fracture. However, if fracture does occur, then our standard multimodal protocol is followed. In some cases, we will electively cut the bone at one or two levels to correct severe deformities and prevent future fractures.
Why choose the International Center for Limb Lengthening for cross-union treatment of congenital pseudarthrosis of the tibia?
Limb lengthening and deformity correction are complex processes. Your doctor at the International Center for Limb Lengthening will take the time to make sure you understand all your options and then will customize your treatment to meet your child’s specific needs. Our patients benefit from our team-centered approach with world-renowned pediatric orthopedic surgeons and specialized physician assistants, nurses and physical therapists. We help patients with congenital pseudarthrosis of the tibia achieve their best possible result.
Chat with a doctor about congenital pseudarthrosis of the tibia
Our doctors hold free monthly chats on various subjects, including congenital pseudarthrosis of the tibia. Click here for more information about our monthly chats.