Fibular Hemimelia
For a printable handout version of most of the content below, please click here.
What is fibular hemimelia?
Fibular hemimelia is a congenital (at birth) limb deficiency where the fibular bone is partially or completely missing in the lower leg. This shortens the affected leg; there is also usually a lower leg deformity or bow and an abnormally positioned foot with missing toes. Although most of the limb abnormalities are concentrated in the lower leg and foot, the entire lower extremity (from the hip to the toes) is affected by this condition. The most inclusive medical term for this condition is post-axial hypoplasia of the lower extremity. This means that one side–the small toe side–of the limb bud was altered resulting in an abnormal growth pattern.
How common is fibular hemimelia?
The incidence of fibular hemimelia is 1 in 40,000 live births. To put this into perspective, the United States of America usually averages about 4,000,000 live births per year. This results in 100 live births with fibular hemimelia per year in the United States.
What are the chances that a second child in the same family will have this condition?
The chances of a second child having fibular hemimelia are the same as the first, 1 in 40,000. Since this genetic mutation is spontaneous, there is no increased risk of having a second child with fibular hemimelia.
What are the chances that a person with fibular hemimelia will have a child with this condition?
A person with fibular hemimelia has a 1 in 40,000 chance of having a child with fibular hemimelia. Since this genetic mutation is spontaneous, there is no increased risk of fibular hemimelia being passed down to the next generation.
What causes fibular hemimelia?
The exact cause of fibular hemimelia is unknown. A spontaneous genetic error occurs during limb bud development in the womb. This growth abnormality occurs during the development of the lower limb bud at six to eight weeks after conception. This “blue print” error resides only in the cells of the limb bud of the developing fetus, not in any reproductive cells from the parents.
How is fibular hemimelia classified?
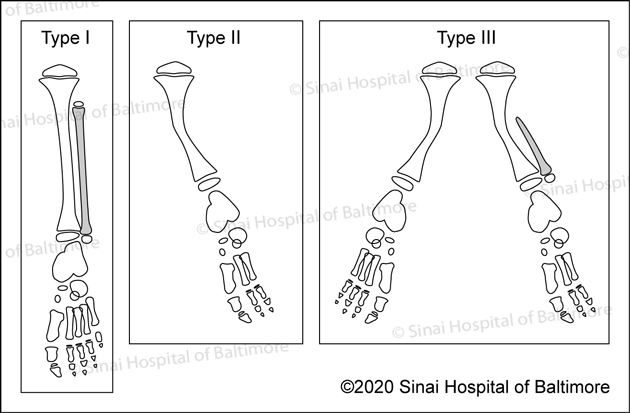 The Coventry and Johnson classification system. Click here for images of all five classification systems.
The Coventry and Johnson classification system. Click here for images of all five classification systems.There are five different fibular hemimelia classification systems used in North America. The earliest one is the Coventry and Johnson classification system. The most commonly used system is the Achterman and Kalamchi classification. The other systems are the Stanitski classification system, the Birch classification system and the more recent Paley classification system. To see illustrations of each classification system, click here.
What are the effects of fibular hemimelia on the lower limb?
The most obvious effects of fibular hemimelia are limb shortening, lower leg deformity or bow, and an abnormally positioned foot with missing toes. However, there are other effects that are more subtle and do not become obvious until later in life. The hip joint can be mildly dysplastic, meaning the cup of the hip joint is shallow. There usually is a difference in length between the normal femur (thigh bone) and the femur with fibular hemimelia. This length difference can be minimal or very significant. The femur usually has an outward twist called external femoral torsion, which can result in an out-toeing gait. The knee is always unstable to some degree due to the absence or abnormality of the ligaments inside the knee joint. The tibia (shin bone) is always shorter on the affected leg with an abnormally positioned ankle and/or foot. The tibia usually has a dimple on the front side of the leg marking the bow or deformity in the tibia.
The fibula (small bone in the lower leg) can be partially or totally absent. When the fibula is totally absent on the X-rays, there is always a fibrous remnant connected to the calcaneus (heel bone) that is very tight and contracted. This fibrous fibula remnant is called the fibular anlage. This tight band of tissue causes the foot and ankle to rotate outwards and the lower leg to grow in a valgus (knocked knee) direction. The foot’s toe down position (equinus contracture) is caused by the malalignment (misdirection) of the ankle joint and the tight heel cord/calf muscle. The ankle joint not only points down, but it also points in an outward direction. This is termed ankle valgus. When severe ankle valgus is present, this gives the appearance that the patient is walking on the inner side of the ankle. The ankle position is a combination of the above stated factors that are all related to fibular hemimelia.
Fibular hemimelia affects the foot in various ways. The most obvious is the absence of the lateral digits or rays. The number of toes present on the foot with fibular hemimelia is extremely variable. Some patients retain all five digits whereas others might have only two digits. There is a common misconception among pediatric orthopedic doctors that the number of toes determines the functionality of the foot. The International Center for Limb Lengthening (ICLL) doctors strongly disagree with this thought process. Every foot with fibular hemimelia is unique and must be examined carefully to determine the functionality. Simply counting existing toes does not allow anyone to predict the function of the foot in the future.
Another foot anomaly that is very consistent in fibular hemimelia is called tarsal coalition. A tarsal coalition is when some of the bones in the foot are not separated. In fibular hemimelia, the ankle bone (talus) is usually fused or coalesced to the heel bone (calcaneus). This results in the absence of the subtalar joint. The subtalar joint is the joint between the ankle bone and heel bone that allows the foot and ankle to rock from side to side. In response to the bones in the foot being fused, the ankle joint will form into a ball-in-socket type of configuration instead of the normal hinge joint.
The ball-in-socket configuration allows for all of the normal ankle motion of toe up (dorsiflexion) and toe down (plantar flexion) along with the side-to-side rocking motion (eversion and inversion) to come from one joint instead of two joints in a normal ankle. The benefit of this ball-in-socket adaptation is to allow all “normal” motion that a normal ankle would possess. The disadvantage of this ball-in-socket ankle joint is the potential for the foot and ankle to angle outward giving a “squashed” foot/ankle appearance that is termed dynamic ankle valgus. Dynamic means that the deformity appears when the joint is stressed by weight bearing. Ankle valgus means a “knocked knee” appearance of the ankle.
The tarsal coalition (fusion of the foot bones) in patients with fibular hemimelia creates a second issue besides the ball-in-socket adaptation of the ankle joint. The ankle bone (talus) and heel bone (calcaneus) are usually fused in an abnormal position with the heel bone (calcaneus) lying next to the ankle bone (talus) instead of underneath the ankle bone. This awkward position of the ankle and heel bones exaggerates the pushed-out appearance of the foot.
In the same way that the number of toes varies among patients, the amount of motion at the ankle joint also varies. Some patients will have normal motion at the ankle while others will have very stiff and immobile ankle joints. Once again, many orthopedists will decide the foot and ankle cannot be reconstructed due to stiffness in the ankle joint. The ICLL doctors strongly disagree. A foot and stiff ankle joint that has correct alignment is a very stable and functional limb. During the reconstruction and lengthening, the amount of ankle motion that a patient starts with is approximately the same ankle motion that the limb will have at the end of reconstruction.
Does every patient with fibular hemimelia have all of the above mentioned abnormalities in the lower limb?
No. The severity of fibular hemimelia has a wide spectrum. For example, one patient may have a predicted 5-cm (2-inch) mild leg length discrepancy (LLD), five toes/rays present on the foot, and mild instability of the ankle. However, another patient might have a predicted leg length discrepancy of 30 cm (12 inches), two or three toes present on the foot, and a very stiff ankle joint. Usually patients with a more severe form of fibular hemimelia will have more effects in the hip joint, femur and knee joint.
What are the goals of treatment in patients with fibular hemimelia?
The goals of treatment are to create a lower limb with a stable hip, knee, and ankle that is equal in length to the opposite lower limb. Also, all deformities in the lower limb are corrected during the treatment. The crucial goal in fibular hemimelia is the reconstruction of the ankle and foot. Contrary to many doctors’ opinions, the amount of length needed does not predict the success of reconstruction or the ability to reconstruct the lower limb. In the same way, the number of toes or rays of the foot does not predict the success of reconstruction or the function of the foot. Most doctors use predicted leg length discrepancy or the number of toes to determine whether to recommend amputation/ablation and prosthetic reconstruction.
In the ICLL’s experience, the success of reconstruction treatment is mainly determined by the foot and ankle reconstruction. This success is not determined by the final ankle motion. The goal is to create a stable ankle and a foot in a normal plantigrade (foot flat on the ground) position. This is achieved with the SUPERankle procedure.
The amount of final ankle motion is usually predetermined by the amount of motion already present at the ankle joint. If a patient presents with a very stiff and deformed ankle, the goal is to achieve a plantigrade position with a stiff but stable ankle. The misconception is that a stiff ankle is a failure of reconstruction. Our doctors believe a stiff ankle in the correct position is a good and functional base for a plantigrade foot. On the other hand, if a patient has a deformed foot and ankle with good ankle motion, then the reconstruction is tailored to both correct the foot and ankle position and maintain ankle motion.
The amount of leg length difference predicted to occur by the end of growth does not determine whether a successful reconstruction is possible. There is no set limit to the amount of overall lengthening that can be performed. However, the overall lengthening amount does determine how many treatments or lengthenings will be needed to equalize the leg lengths at maturity. For example, if a 2-year-old boy has a 2.5-cm (1-in) leg length discrepancy, his predicted leg length difference at maturity would be 6.5 cm (2.6 in) when calculated using the Multiplier method. This amount of lengthening could be accomplished with one lengthening procedure.
On the other hand, a 2-year-old girl with a 6-cm (2.4-in) leg length difference would be predicted to have a 14.5 cm (5.7 in) difference at the end of growth. This amount of difference would require two lengthenings to accomplish about 11 to 12 cm (4.3 to 4.7 in) of lengthening. The remaining 2.5 to 3.5 cm (0.98 in to 1.4 in) of difference can be corrected either by a smaller third lengthening at the end of growth or a slowing down procedure of the long leg at the age of about 10 or 11 years. These types of strategies will be explained in greater detail below. The main point is that the total amount of length needed does not determine whether the reconstruction can be performed, but rather how many interventions or surgical procedures will be needed to successfully complete the reconstruction.
What is the typical treatment for a patient with fibular hemimelia?
The patient with fibular hemimelia is usually seen in the first year of life. At the initial visit, X-rays are obtained to evaluate the exact configuration of the skeletal anatomy of the lower legs and to determine the amount of discrepancy in length between the legs. The current leg length discrepancy is used to predict the final leg length discrepancy at the end of growth. This predicted leg length discrepancy will allow the doctor to create a general treatment plan. Also, the predicted amount of limb lengthening required determines the number of surgical procedures required.
The initial clinical exam identifies the shape and position of the foot and ankle. Also, the range of motion and stability of the hip, knee and ankle are assessed and recorded. At this point, our doctors look for a concurrent congenital femoral deficiency and hip joint shallowing in the X-rays. Clinically, the doctor assesses the stability and range of motion of the knee joint. As stated above, the hip and knee are always involved to some degree in fibular hemimelia. If the involvement of the hip and knee are severe, then the overall reconstruction plan is altered by planning either concurrent hip/knee reconstruction or sequential reconstruction. Most commonly, the significantly involved hip and knee would be addressed first between the ages of 18 and 24 months with the SUPERhip/SUPERknee procedure. (The nickname “SUPER” is used for several reconstructions of congenital limb deficiency. Each reconstruction consists of multiple procedures or steps to achieve the comprehensive joint reconstruction.) The ankle reconstruction, called the SUPERankle procedure, would then occur 6 to 12 months after the hip and knee reconstruction.
However, if the growth abnormality is mainly concentrated in the lower leg, then the SUPERankle reconstruction is performed between the ages of one and two years. The initial surgery concentrates on positioning the foot and ankle in a stable or corrected position while concurrently correcting the bowing in the lower leg. The second stage would be a 5-cm (2-inch) lengthening of the tibia performed 12 to 24 months after the first surgery.
The number of subsequent lengthenings is determined by the overall predicted lengthening goal. The subsequent lengthenings are performed at intervals of 4 to 6 years apart for a total of up to three lengthenings for the most severe types of fibular hemimelia. The first lengthening usually achieves a 5-cm (2-inch) gain in length. Subsequent lengthenings can achieve between 5 and 7 cm (2 and 2.8 inches) of length.
For all patients who will undergo lengthening, we may recommend that they undergo a prophylactic anterior compartment fasciotomy to decrease the risk of compartment syndrome and create a calf that looks larger in diameter. To see an illustration of this surgical technique, click here.
What other types of surgeries can be expected during the treatment of fibular hemimelia?
After the initial reconstruction of the foot and ankle, the lower extremity can grow into a valgus or “knocked knee” position due to abnormal growth at the growth plates of either the distal (lower) femur or proximal (upper) tibia. The “knocked knee” deformity has also been attributed to the shape of the distal femur or the tethering effect of the residual scar-like fibular band called the fibular anlage. Genu valgus (knocked knee position) is treated by either straightening the bone during lengthening or performing hemiepiphysiodesis (guided growth).
Hemiepiphysiodesis is a minor procedure in which a small, two-hole plate is placed over the growth plate on the inner or outer aspect of the leg. This plate acts like a bracket that slows the growth on one side of the growth plate causing the bone to gradually turn as it grows, which corrects the knocked knee deformity. Once the leg is straight, the plate is removed. The placement and removal of the plate is performed during a brief outpatient surgery. The plates are called eight-Plates (manufactured by Orthofix) or Peanut Plates (manufactured by Biomet).
Sometimes a smaller revision surgery is required after the SUPERankle procedure. After the initial correction of the foot and ankle with the SUPERankle procedure, the foot can shift back to the outside. This gives the appearance that the child is walking on the inside ankle bone. This phenomenon can occur soon after the SUPERankle procedure when the child returns to weight bearing or can gradually appear as the child continues to grow. This recurrent type of deformity is unusual.
If the foot and ankle deformity returns soon after the initial procedure, then it means that an underlying bony deformity was either under corrected or unmasked by the initial reconstruction. One must understand that the initial reconstruction is a very complex set of procedures that is unique for each child. The deformity related to fibular hemimelia is the combination of contracted soft tissues and abnormally formed joints of the ankle and foot. This unmasked deformity or recurrence can be addressed with a smaller revision surgery that requires a bone cut in the distal tibia or between the ankle and heel bone. Usually the leg is placed in a cast for 4 to 6 weeks to heal, and then the child is allowed to wear regular shoes.
The foot and ankle deformity that gradually reappears during early adolescence is addressed at the final surgical intervention, which usually occurs between 12 and 16 years of age. At the final surgical reconstruction, the leg lengths are equalized with a lengthening from the upper tibia, and the foot/ankle position is corrected from the lower tibia. After this reconstruction is complete, the correction is permanent since the patient is nearing the end of growth.
What is the SUPERankle procedure?
The SUPERankle procedure is a comprehensive release of the contracted soft tissues around the ankle joint with osteotomies (bone cuts) of the midshaft tibia (shin bone), distal tibia (right above the ankle) and hindfoot (ankle and heel bones). This procedure aligns the foot and ankle and corrects the patient’s downward and outward foot deformity. Click here for a detailed explanation and surgical illustrations of the SUPERankle procedure.
What happens in the later lengthening stage?
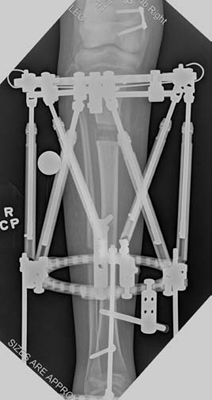
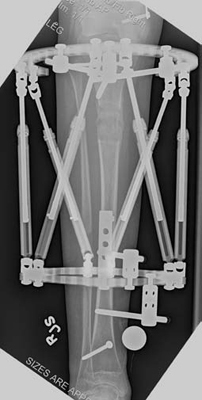
If the patient is undergoing lengthening for fibular hemimelia, then a Taylor spatial frame (TSF) external fixator is used. During the lengthening phase, the patient or parent adjusts the TSF on a daily basis to perform the lengthening and deformity correction. The patient is seen every two weeks for clinical and X-ray examination here at the International Center for Limb Lengthening (ICLL) in Baltimore, Maryland.
The lengthening phase of the treatment lasts for 2 to 3 months. Once lengthening is completed, the adjustments stop and the consolidation or healing phase begins. The consolidation phase can last from 2 to 4 months. During this period, the TSF remains on the leg, and the patient will have X-rays taken once a month. These X-rays can be taken at another center that is close to the patient’s home and then sent to the ICLL. Clinic visits at the ICLL are not necessary during the consolidation phase unless issues or problems arise.
What is the typical tibial lengthening protocol for fibular hemimelia?
One or multiple tibial lengthenings are performed when patients have a significant leg length discrepancy. The amount of length gained during a single lengthening treatment usually is determined by the new bone quality or the motion of the joints above and below the lengthening site. The amount of lengthening will be limited if the patient has poor bone quality or stiffness of the joints with loss of motion. In patients younger than 6 years of age, the maximum length gain during a single lengthening is 5 cm (2 inches). The total amount of lengthening in a younger patient is limited to avoid extreme pressures on the growth plate that can cause premature closure of the growth plate and loss of potential or “natural” growth. Older patients can acquire more length in a single treatment–between 6 and 7 cm (2.4 and 2.8 inches).
 Emma wearing an external fixator in the pool.
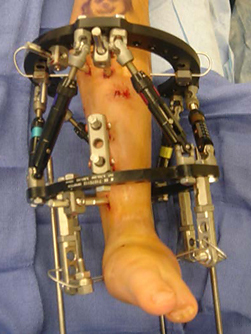
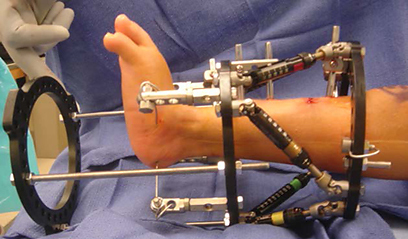
Emma wearing an external fixator in the pool.Typically the patient is admitted to the hospital on the day of the lengthening surgery. A circular external fixator is placed on the lower leg and foot of the involved side. The type of external fixator used is usually the TSF. The foot is always included in the TSF to ensure stability of the ankle joint and to maintain the proper foot position during the distraction or lengthening phase of the treatment. The tibia is cut through one or two small incisions after the TSF is applied. The TSF stabilizes the cut bones and maintains alignment.
After surgery, the patient stays at the hospital mainly for pain control and close observation of the neurovascular status of the limb. The initial hospitalization is usually 3 to 4 days. Postoperative pain is controlled with epidural analgesia or intravenous pain medicine on a patient control anesthesia (PCA) machine. During the first two days of hospitalization, the pain control is fine-tuned with adjustments in the medicine doses or route of delivery. Also, physical therapy begins with gentle range of motion of the hip and knee on the involved side. The main goal in this part of physical therapy is to maintain full knee extension and to gain knee flexion to at least 60 to 70 degrees. The second aspect of physical therapy is to begin mobilization of the patient. This starts with simply sitting on the side of the bed or transferring to a wheelchair. Mobilization increases over the hospital stay to standing transfers and ambulation with a walker or crutches.
To lengthen the leg and correct the deformity, the patient or parent must adjust the struts on the TSF daily. During the first 5 to 7 days after surgery, the TSF is not adjusted. This allows the bone to recover from surgery and to begin to heal. After bone healing starts, the external fixator is activated and the lengthening begins. The lengthening phase is the time period where the TSF is adjusted on a daily basis by pulling the bone ends slowly apart (between 0.5 mm and 1.0 mm / day), which results in new bone formation. The lengthening phase lasts for 2 to 3 months depending on the amount of length needed. Younger patients can put as much weight as they can tolerate on the operated leg. Older and larger patients are kept at 50% weight bearing during the lengthening phase.
During hospitalization, a social worker will meet with the family to assess needs and to make arrangements for equipment (walker, wheelchair, etc.). Special transportation is also assessed, but it is rarely needed with the lower leg external fixation devices used for fibular hemimelia.
 Emma as a young girl wearing an external fixator.
Emma as a young girl wearing an external fixator.The patient is discharged from the hospital after the pain medications have been converted to an oral type of medicine, the patient is tolerating a regular diet with good fluid intake, the family is comfortable with the specifics of daily care, and the patient clears the physical therapy assessment for safe mobilization and transfers. Upon discharge, the family will have a supply of pain medication, antibiotic medication and dressings. Contact numbers are provided to the family so that questions and concerns can be addressed at any hour of any day during treatment.
After discharge, the outpatient portion of the lengthening treatment begins. This includes outpatient physical therapy five days a week as well as a daily exercise and stretching program. Office visits are necessary every two weeks at the International Center for Limb Lengthening. These follow-up examinations prevent major complications during this critical lengthening phase. Each office visit includes a clinical examination of the operative leg and frame along with obtaining X-rays to assess the bone’s position and length gained.
Once the lengthening phase is completed and the planned length gained, the consolidation or healing phase begins. During the consolidation phase, the TSF remains in place for stabilization but no further adjustments are performed. Usually the consolidation phase lasts from 2 to 4 months, and patients are allowed full weight bearing. Office visits are not necessary unless concerns or problems arise. Instead, X-rays are obtained every 4 to 6 weeks in the patient’s hometown and sent to the ICLL for the doctor’s review. The family is contacted via phone or e-mail to discuss the results of the X-rays and the next step in treatment.
Once the monthly X-rays show adequate healing of the new bone, the TSF removal surgery is scheduled in the following 2 to 4 weeks. This surgery is usually an outpatient procedure. After the TSF is removed, a long leg cast is applied for 2 to 4 weeks. The post-removal cast protects both the new bone and the pin holes left by the external fixator from potential fracture. Usually the patient may bear full weight in the post-removal cast.
Four weeks after TSF removal, the cast is removed and converted to a cast brace that may be weaned according to the patient’s comfort. A gradual return to normal activities occurs over the following 2 to 3 months. Contact sports to include soccer, lacrosse and football may be resumed 6 to 8 months after frame removal. Subsequent visits become annual or biannual office visits to assess the growth of the limb, recurrent limb length discrepancy, recurrent alignment problems and future reconstructive plans.
What are the physical therapy requirements during the lengthening process?
Physical therapy is the most important aspect of the lengthening process. Without proper physical therapy, the lengthening goals will not be achieved and major complications will occur. Therefore, physical therapy requirements are very strict. The patient undergoing tibial lengthening must receive physical therapy 5 days per week while at the same time performing an exercise and stretching program at home. The physical therapy continues at this level of intensity for the duration of the distraction phase (2 to 3 months depending on the planned amount of lengthening). Parents and patients must stay in Baltimore for at least 2 to 4 weeks to begin therapy at the ICLL. During this initial therapy, the parents are taught home exercises and stretching techniques that their child must perform every day. Also, the parents are able to observe the therapy sessions and the therapists’ techniques.
 Gracie learning to use a walker in physical therapy.
Gracie learning to use a walker in physical therapy.The physical therapy department at the ICLL is headed by Anil Bhave, PT who has tremendous experience in limb lengthening and reconstruction therapy. His team provides land and water therapy for patients undergoing lengthening. The on-site therapy center includes inpatient and outpatient therapy gyms and a state-of-the-art gait analysis laboratory. Our therapy team has the most experience in terms of limb lengthening and limb reconstruction.
During the distraction phase, the ideal situation is to perform all physical therapy at the ICLL in Baltimore. This will require a stay of 2 to 3 months in Baltimore. Once the distraction phase is completed, the therapy requirements significantly decrease. At that point, the family may return home and their therapy transitions to a local therapist with guidance from the therapists at the ICLL.
However, if the 2- to 3-month stay is not feasible for the family, then the next best option is to have the patient begin therapy at the ICLL for 2 to 4 weeks. After 2 to 4 weeks of therapy at the ICLL, the family has a better understanding of what constitutes adequate therapy. Also, with guidance from both the therapists and the clinical staff, the families become familiar with the external fixation care and maintenance. Before leaving Baltimore, the ICLL therapist creates the therapy plan with the approval of the attending physician and communicates this plan with the local therapist. Even if the patient has returned home during the lengthening phase, the office visit for clinical and X-ray evaluation that occurs every 2 weeks is still mandatory.
If the family plans to return home immediately after the hospital stay, the patient must undergo at least one week of therapy at the ICLL. This is to allow the therapy team time to teach the family the lengthening stretches and prepare them for the transition to the local therapist. Again, the family choosing this strategy must still return every two weeks for the clinical and X-ray evaluations at the ICLL clinic. We do not recommend this strategy due to the increased complication rate and the decreased overall length gain of the patients when compared with patients who have chosen to perform most of the therapy at the ICLL.
The relationship between the patient and the physical therapist is very important while the family is in Baltimore and becomes even more important when the family and patient return home. The therapists are the remote eyes and ears of the physician. During the daily therapy, if any concerns or complaints arise, the therapist notifies the surgeon immediately for a recommended solution or makes sure that the patient is seen in the office for a clinical check. After the patient returns home, the ICLL therapist will intermittently check on the patient’s progress and discuss the therapy with the local therapist. If there is a significant therapy issue, the individual therapist or Mr. Bhave notifies the local therapist and provides additional instructions.
Will the family have an opportunity to learn more about the external fixator and other postoperative care?
Families will have a teaching session that will provide a general overview of external fixation care and management along with specific instructions on the type of external fixation device that will be applied. The education and instruction on frame care and maintenance continues through the entire hospitalization. The initial dressing change and pin care starts the second day after surgery. The family and patient learn the proper pin care methods and participate from the very beginning. This is a very important step that allows the patient to overcome the fear and anxiety of wearing an external fixator.
How is the lower extremity deformity and leg length discrepancy managed before or between reconstructive treatments?
Before a lengthening or reconstruction is performed, the lower leg is treated with a brace and a shoe lift as needed. The brace provides stability and the shoe lift provides additional length to the short limb. Usually a lower leg brace or ankle foot orthosis (AFO) is not needed before the initial reconstruction. Sometimes, if the deformity is severe and the leg length discrepancy is greater than 5 cm (2 inches), an AFO is used to support the foot and ankle during shoe wear.
Typically, after the initial foot and ankle reconstruction is completed, an AFO and appropriate-sized shoe lift are used temporarily. These assistive devices are usually discontinued after the patient has completed the postoperative physical therapy and the bone has healed.
In between surgical interventions, most legs do not require bracing. If a patient’s leg length discrepancy is greater than 2 cm (3/4 of an inch), a shoe lift can be used. Again, an AFO is used if the residual leg length discrepancy is greater than 5 cm (2 inches).
What is the strategy for shoe lifts?
A shoe lift is used if the leg length discrepancy is greater than 2 cm (3/4 of an inch). The height of the lift is calculated by subtracting 1 cm (0.4-in) from the total discrepancy. For example, a patient with a 4.5-cm (1.8-in) leg length discrepancy would be given a 3.5-cm (1.4-in) shoe lift. This 1-cm (0.4-in) reduction prevents the lift from catching on the ground and allows for better clearance of the shorter leg during walking.
 Primo playing on the monkey bars while wearing a shoe lift.
Primo playing on the monkey bars while wearing a shoe lift.The reason a patient with a leg length discrepancy wears a shoe lift is to prevent an ankle contracture in a toe-down direction (equinus contracture) and to improve the patient’s gait and posture. If a person with a significant leg length discrepancy does not use a shoe lift over the period of 15 to 20 years, the person may experience long-term problems such as back pain, hip joint arthritis, and knee joint arthritis. However, these long-term problems will not occur in young children if they do not use their lifts all the time.
The International Center for Limb Lengthening doctors usually recommend that the child use the prescribed lift on their most commonly used shoe (school shoe or play shoe). It is perfectly fine for a child to spend a significant portion of the day barefooted or not using a shoe lift as long as the ankle range of motion remains normal. This is especially important during the summer when sandals and flip flops are very popular.
The lift should not be used on athletic shoes or cleats. For sports, the feet should be shoed individually and the smaller fibular hemimelia foot should have a smaller, well-fitted shoe with no lift. To learn more about shoe lifts, see our video “The Art of Shoe Lifts.”
Will a child with fibular hemimelia learn to walk?
This is a very common question with a very easy answer—the children do just fine and nothing stops them from walking. Even with a severe foot and ankle deformity and a leg length discrepancy, a child will adapt and walk usually between 12 and 16 months of age. If weight bearing on the affected limb appears to be placing forces across the foot and ankle that push the foot into a more deformed position, then a small lower leg brace will be used as mentioned above. This is only a temporary problem because the initial reconstruction is performed at the age of 18 to 24 months.
Why choose the International Center for Limb Lengthening for treatment of fibular hemimelia?
Limb lengthening and deformity correction are complex processes. Our pediatric orthopedic team has extensive experience in limb lengthening and reconstruction and treating this specific condition. Your doctor will take the time to make sure you understand all your options and then will customize a treatment plan to meet your child’s specific needs.
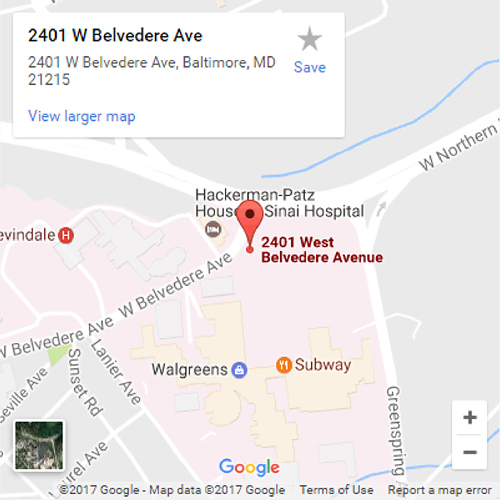
The International Center for Limb Lengthening at the Rubin Institute for Advanced Orthopedics at Sinai Hospital was specifically designed for the complex treatment of limb deformities. The building has physician offices, six operating rooms specially designed for limb lengthening procedures, physical therapy gyms and a gait lab all right on site at Sinai Hospital. An apartment-style housing facility, the Hackerman-Patz House, was built across the street from the hospital to accommodate families during treatment. The Baltimore Ronald McDonald House also is available for families to stay at while a child undergoes treatment, and it provides a shuttle service to the ICLL. Our patients find both housing options provide a supportive family atmosphere.
Our patients also benefit from our team-centered approach with world-renowned pediatric surgeons, specialized physician assistants, nurses and physical therapists, a child life specialist, and a nurse educator. We also have orthopedic technologists, X-ray technologists and full-time staff pediatricians in the pediatric inpatient unit. We help patients with fibular hemimelia achieve their best possible result.
Handout
Videos
Chat with a doctor about fibular hemimelia
Our doctors hold free monthly chats on various subjects, including fibular hemimelia. Click here for more information about our monthly chats.