Perthes Disease
For a printable handout version of the content below, please click here.
What is Perthes disease?
Perthes disease, also called Legg-Calve-Perthes Disease, occurs in children when blood stops flowing to the femoral head, which is the ball of the ball and socket joint of the hip. Like any tissue that loses circulation, the bone of the hip dies. Death of bone due to a lack of blood supply is called avascular necrosis (AVN) or osteonecrosis. When adolescents have avascular necrosis of the hip, it is called Adolescent AVN; in children, it is called Perthes disease.
The normal reaction of the body to dead tissue is to remove it and replace it with living tissue. Gradually, the dead bone of the femoral head is removed by special cells in the bone called osteoclasts. At the same time, new bone is added by special cells called osteoblasts. If this demolition and reconstruction occurred in a completely coordinated fashion, there would be no problem. Unfortunately, the removal of bone weakens the femoral head and the bone in the femoral head cartilage (the outer coating of the joint) becomes deformed because of lack of bony support underneath. Fortunately, the cartilage on the outside of the femoral head is alive and able to grow. This is analogous to the removal of the support beams of a building by one construction crew and the subsequent replacement with new support beams the next day by another crew. In the interim, the roof of the building collapses.
What factors affect Perthes disease?
The factors that affect the final outcome are the age of the patient, sex of the patient, the range of motion of the affected hip joint, the amount of necrosis (dead bone) or involvement of the femoral head, the stage of the disease process, and X-ray evidence of “containment.” These factors can help predict the likelihood of a poor or good outcome. With this information, the correct treatment can be selected from the various options.
Age of the Patient
The younger the patient, the better the outcome is in Perthes disease. A better outcome is defined as a round femoral head (hip ball) in a matching acetabulum (hip cup). However, Perthes disease not only affects the shape of the femoral head; it also significantly affects the growth of the femoral neck (neck of the thigh bone) and femur (thigh bone). Every patient with Perthes disease will have a slowing of the growth in the upper end of the femur (thigh bone). This can result in a clinically significant or problematic leg length discrepancy (more than 2.0 cm or ¾ inch) or a very short femoral neck (neck of the thigh bone). If a young patient has Perthes disease, the disease has more time to slow the growth of the femoral neck and femur before the patient is done growing. As a result, younger patients end up with better hip joints but possibly shorter legs and/ or femoral necks. Older patients end up with more hip joint deformity or misshapen femoral heads, but they have a small leg length discrepancy or a relatively normal femoral neck length. The definition of “young” and “old” in Perthes disease is not set in stone. The International Center for Limb Lengthening uses the following definitions:
Younger patients have a better chance of a successful outcome with non-operative or minimally invasive procedures. Older patients require more aggressive treatment, which usually means more complex or involved surgical treatment. The reasons for the above break down of ages and outcomes have to do with the fact that younger patients have more growth and healing potential then the older patients. The more growth the child has remaining, the more remodeling/healing can occur of the femoral head and the cup that it fits inside. Additional time spent remodeling/healing will allow the femoral head and cup time to repair and to become round.
Sex of the Patient
Girls fare worse than boys because they become skeletally mature at a younger age than boys. Girls finish growth in the femur (thigh bone) at an average age of 14 years while the femur in boys is done growing at age 16 years.
Range of Motion of the Affected Hip Joint
The range of motion of the involved hip joint is the most important factor. This was noted from the very first time this disease was identified by Dr. Arthur Legg and Dr. Jacques Calvé (1910). Motion is essential to maintain the roundness of the femoral head. During the process of Perthes disease, the inner bone that supports the round cartilaginous femoral head begins to fail as the “dead bone” is absorbed by the body. The loss of this inherent stability of the femoral head creates a situation where the femoral head “softens” and takes on the characteristics of a ball of molding clay or a water balloon.
If the hip motion is lost and the soft femoral head is stuck in one position, then the edges of the hip acetabulum (hip cup) push down on the soft femoral head and change the shape of the hip ball. This femoral head deformation causes a mismatch in the shape of the hip ball and cup which leads permanent loss of motion, wear and tear on the joint, impingement pain, and eventual arthritis. Impingement pain occurs when the hip no longer moves freely (it gets “stuck”).
On the other hand, if the hip joint motion is maintained, then the soft femoral head is molded like a ball of clay within the hip cup and remains round or spherical. It is important to realize that no matter which treatment is provided, the femoral head shape and size will always change to some degree. Again, the definition of success in Perthes disease is to complete treatment with a round or spherical femoral head that “fits” into the hip cup and provides adequate hip range of motion.
What is considered good or adequate range of motion of the hip is a common question. The International Center for Limb Lengthening considers the following range-of-motion parameters acceptable during the treatment of Perthes disease:
Amount of Necrosis or Involvement of the Femoral Head
This is a very important factor. Necrosis means that the bone has become dead tissue. This is a measure of the percentage of bone in the femoral head that has died. The greater the amount of bone that has died, the poorer the final outcome (or the higher the risk of a poor final outcome) will be. If the central, core part of the femoral head is involved, the support structure of the femoral head is very vulnerable. This can be compared to support beams that hold up a roof or ceiling. The more support beams that are “rotten,” the more likely the structure will fail and the roof will collapse.
In terms of involvement, the amount of hip necrosis is usually defined as greater than or less than 50% of the femoral head. This means that if only a very small area of bone necrosis is identified, then the risk of further collapse and problems is very small. This means that if only a very small area of bone necrosis is identified, then the risk of further collapse and problems is very small. Unfortunately, the majority of Perthes cases involve more than 50% of the femoral head.
Stage of Disease Process
The Perthes “process” can be broken into nine separate stages that each hip with Perthes goes through. Several classification systems already exist in the literature, but the stages provided below were created based on the many patients treated at the International Center for Limb Lengthening. Below are X-ray examples of the stages of progression in Perthes disease. The examples below are from three different patients and provide the best example of each stage. Stage 1 is the only image of that patient. Stages 2 through 6 show the same patient and stages 7 through 9 show the same patient.
- Stage 1: Precollapse
No height difference in the core of the femoral head as compared to the opposite side.

- Stage 2: Early Collapse
More than 75% of the height of the core of femoral head as compared to the opposite side.

- Stage 3: Mid-Collapse
Between 50% and 75% of the height of the core of femoral head as compared to the opposite side.

- Stage 4: Late Collapse
Less than 50% of the height of the core of femoral head as compared to the opposite side.

- Stage 5: Early Fragmentation
Less than 50% of the femoral head demonstrates fragmentation of the core of bone.

- Stage 6: Late Fragmentation
More than 50% of the femoral head demonstrates fragmentation of the core of bone.

- Stage 7: Early Reconstitution
Less than 50% of the femoral head demonstrates new bone formation (reconstitution).
- Stage 8: Late Reconstitution
More than 50% of the femoral head demonstrates new bone formation.

- Stage 9: Healed/Reconstituted
The femoral head demonstrates reconstitution and a solid core of bone.

The purpose of defining the stage of the disease is to give the parents a timeline of where their child is along the “Perthes process.” Please note that although there is a significant variability in this timeline, most Perthes patients complete this process within 18 to 24 months from the start of the hip symptoms. Treatment that is begun before the late fragmentation stage (stage 6) is more likely to have a successful outcome than treatment begun in the later stages. If the patient is not doing well with a current treatment plan and has loss of hip motion and stiffness, then an aggressive intervention needs to be started before the late fragmentation stage. This stage usually correlates with a change in the shape of the cartilaginous part of the femoral head.
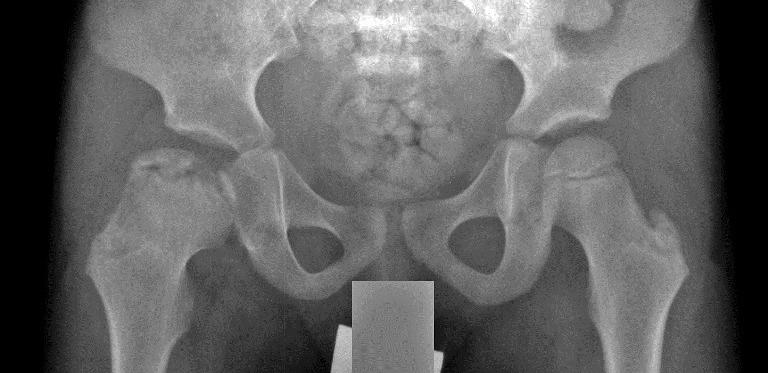
X-Ray Evidence of Hip “Containment”
Hip containment is defined as the ball of the hip joint being properly matched and congruent within the hip cup. When the cartilaginous part of the femoral head (hip ball) collapses, the femoral head will migrate or shift out of the socket. When the femoral head migrates or shifts, it is termed “loss of containment” or “subluxation of the hip joint.” The most consistent way that doctors use to determine whether the hip joint has migrated is to look for a break in Shenton’s line and increased medial joint space on an X-ray.
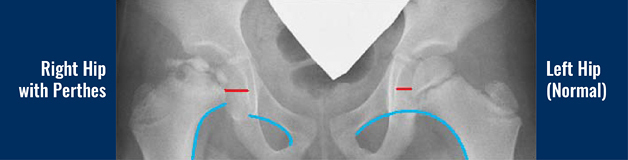
This X-ray example shows a hip that has lost containment and has migrated outward and upward. The blue line represents Shenton’s line, which should normally be a continuous, unbroken line, as seen on the left hip. Also, the outward or lateral migration of the hip is seen by observing the medial joint space as represented by the red lines. The red line of the right hip is larger than the red line of the left hip. This means the right hip has shifted to the outside or lateral.
How are these factors used to classify risk?
The International Center for Limb Lengthening uses the factors above to classify the hips into low-risk, gray zone, or high-risk categories. Once the hip has been classified, then the appropriate treatment plan can be started:
- Low-risk hips are usually found in younger patients. These hips have good range of motion with intermittent or minimal symptoms. The majority of these hips require non-operative treatment or occasionally minimally invasive treatment (treatments are described in the next section).
- Gray zone hips are found in young patients who have more symptoms or loss of hip motion or in older patients who have maintained good hip motion. These hips require close follow-up with aggressive stretching exercises (non-operative treatment) or immediate minimally invasive treatment to expedite the healing process and get the patient back on the right course.
- High-risk hips are found in older patients who have loss of hip motion or in any patient who presents to clinic in the later stages of the disease with loss of containment and a stiff hip. These hips require aggressive surgical treatment.
What are Perthes treatment options?
Perthes treatment options can be broken into three categories: non-operative treatment, minimally invasive surgical treatment and aggressive surgical treatment.
Non-surgical treatment
Non-surgical treatment for Perthes consists of daily stretching exercises performed at home once or twice daily. We call the exercises “Perthes Stretching Exercises” and they consist of five basic hip stretches that maintain the essential hip motion that is needed for a successful outcome.
Although the hip stretching exercises are the non-surgical treatment option, these same stretches are a part of all the Perthes treatment plans at our center. No matter what treatment option we use, the hip motion must be restored and maintained to have a successful outcome. In addition to the Perthes exercises that are done at home, patients may also need formal physical therapy. However, this physical therapy should be based on aggressive stretching exercises. We recommend that all patients find a physical therapist close to where they live so that they can work with this person throughout the treatment process.
 Scottish Rite Brace
Scottish Rite BraceOccasionally, nighttime bracing is used along with the Perthes exercises. The brace is called a Scottish Rite brace. This brace helps to maintain the range of motion in the abducted (“snow angel”) position.
If non-surgical treatment is chosen, the child returns to clinic for follow-up visits every 4 to 6 weeks during the initial 6 months of the Perthes process. After the critical stages of fragmentation and early healing, the clinic visits become less frequent and occur every 6 to 12 months until growth is completed. As far as activity limitations, normal activity is okay, but children should avoid “big” runs and jumps (e.g., they should not jump off the jungle gym or out of a car). As the Perthes process progresses, the activity level can be increased as long as the hip range of motion is maintained, and the child does not feel any pain in the hip.
Minimally Invasive Surgical Treatment
There are two minimally invasive surgical treatments:
- Arthrogram and Botox Injection
While the child is under anesthesia, the doctor will conduct a brief evaluation and exam of the hip. With the child asleep and completely relaxed, the true motion of the hip can be determined. At the same time, an arthrogram (injection of a dye into the hip joint) is performed. The dye coats the cartilage and allows the true shape of the cartilaginous part of the femoral head to be seen and examined under live X-ray. A live X-ray means that the X-ray machine captures images of the hip as the hip is moved in all directions. This live X-ray with the dye shows the cartilaginous part of the femoral head while a normal X-ray shows only the bony part at the center of the femoral head.A Botox solution is injected into the inner thigh muscles. This Botox injection will relax the inner thigh muscles and will allow the hip to have a better range of motion in the hip abduction position (snow angel position) during Perthes exercises and during physical therapy. Botox injections are regularly used to treat other muscle conditions where the muscles are too tight. The effects of the Botox injection are not permanent, and full muscle strength returns in a period of about 3 months.
- Small-Diameter Core Decompression and Injection of Bone Stem Cells into the Femoral Head
When we perform the arthrogram and Botox injection, we may also decide to simultaneously perform a small-diameter core decompression and inject bone stem cells into the femoral head. During small-diameter core decompression, a wire with a 1 to 2 mm diameter is used to make small holes in the femoral head to stimulate the healing process of the core of bone inside the femoral head. The wire is inserted through a small incision and is then guided through the femoral neck into the center of the femoral head.
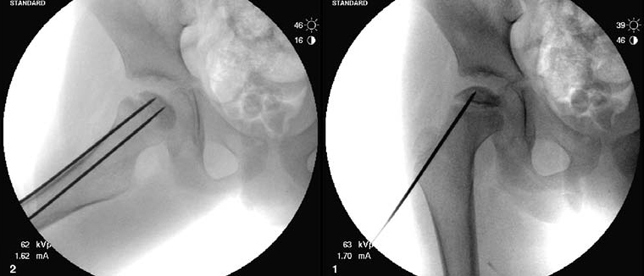
The idea behind core decompression is that we make these small holes to stimulate the bone to expedite the healing process and to stimulate the body to make new bone. The main concern of this type of procedure is the potential harm that could be caused by the wires crossing the growth plate in the upper thigh bone. After a review of 30 cases of Perthes disease treated by small-diameter core decompression, there was no evidence of harm to the growth plate. This same data showed a 70% success rate for this procedure. Success was defined as the hip requiring no further treatment for Perthes disease.
 To improve the success rate, bone stem cells are injected into the femoral head at the same time that the small-diameter core decompression is performed. The bone stem cells are taken from the child and then injected into the femoral head. Since they are taken from the child and are not from another person, they are called autologous bone stem cells. This means the bone stem cells are only from the child, with no synthetic or donor cells involved. The bone stem cells are harvested through a simple needle aspiration from the part of the hip bone that is at the waistline (iliac crest). The bone marrow aspiration is then placed in a machine that spins and concentrates the bone stem cells. A bone channel is created in the femoral neck through a small incision, but the bone channel does not cross the growth plate. A special needle is then inserted into the core of the femoral head, and the bone stem cells are injected. The goal is to inject the bone stem cells right into the area where the bone tissue has died.
To improve the success rate, bone stem cells are injected into the femoral head at the same time that the small-diameter core decompression is performed. The bone stem cells are taken from the child and then injected into the femoral head. Since they are taken from the child and are not from another person, they are called autologous bone stem cells. This means the bone stem cells are only from the child, with no synthetic or donor cells involved. The bone stem cells are harvested through a simple needle aspiration from the part of the hip bone that is at the waistline (iliac crest). The bone marrow aspiration is then placed in a machine that spins and concentrates the bone stem cells. A bone channel is created in the femoral neck through a small incision, but the bone channel does not cross the growth plate. A special needle is then inserted into the core of the femoral head, and the bone stem cells are injected. The goal is to inject the bone stem cells right into the area where the bone tissue has died.The combination of performing a core decompression to stimulate healing and inserting bone stem cells increases the chances of the bone healing and the symptoms resolving. The International Center for Limb Lengthening has seen a more than 95% success rate when the small-diameter core decompression is combined with the bone stem cell injection. Again, success is defined as a resolution of the Perthes process with no further surgical treatment, and that the femoral head is maintaining a round, spherical shape. Although promising, the procedure and results are preliminary, and further follow-up is needed to determine the exact predictability. It is also difficult to determine whether the bone stem cells actually speed up the process of healing. In our experience, the best-case scenario is rapid healing of the core of bone that can be seen on an X-ray within 8 to 12 weeks. The worst-case scenario is that new bone is not created, and the collapse of the femoral head continues.
The combined core decompression and stem cell injection is an outpatient procedure, meaning that the child does not need to spend the night after surgery in the hospital. The child recovers from the mild soreness within 10 to 14 days. After the procedure, a Scottish Rite brace is worn during the day and at night. Eventually, when the range of motion of the hip is maintained and stabilized, the brace is worn only at night. After the core decompression and stem cell injection, the child returns to the clinic for follow-up visits every 4 to 6 weeks during the six months after surgery.
It should be emphasized that the basic stretching exercises are still very important and still need to be performed 2 to 3 times per day after any of the minimally invasive treatments described in this section. If the hip range of motion is not gained and maintained, then the treatment will fail.
Aggressive Surgical Treatment: Hip Distraction
If the hip has not improved or stabilized after more conservative treatments, or if the hip is classified as being high risk, then more aggressive treatments are used. There are different types of surgeries that cut the bone of either the pelvis or the upper femur in order to place the femoral head within the hip cup. These types of operations are called pelvic and femoral osteotomies. Although these procedures may be used as part of the surgical treatment, we rarely use them as the primary surgical treatment. The International Center for Limb Lengthening’s primary procedure for severe Perthes disease is hip distraction treatment.
What are the major phases of hip distraction treatment for Perthes disease?
Hip distraction treatment is made up of five phases. (You may find it helpful to refer to our hip distraction timeline.) During phase 1, the doctor performs soft tissue releases of the contracted hip joint, performs an arthrogram, and applies an external fixator to the hip and upper leg. Phase 1 might also include small-diameter core decompression and bone stem cell injection (described in the “Minimally-Invasive Surgical Treatment” section). During phase 2, the external fixator is used to slowly and gently pull the femoral head 5 to 10 mm away from the cup. This prevents any further pressure or force on the soft femoral head. The external fixator also holds the femoral head in the cup and maintains perfect containment. The external fixator is removed during phase 3. During phase 4, the child wears a brace/pillow, continues Perthes exercises at home and physical therapy sessions, and attends follow-up appointments at the Rubin Institute. The progress with the hip is monitored and maintained during stage 5.
- Phase 1 of Hip Distraction: Surgery to Release Soft Tissues and Apply the External Fixator
- The surgery is performed under general anesthesia and lasts 3 to 4 hours. While the child is under the effects of anesthesia, an epidural catheter is placed in the lower back. After surgery, medication is given through the epidural catheter to control pain.
The surgery consists of soft tissue releases (tendon releases) in the groin and inner thigh, an arthrogram of the hip joint, and the application of an external fixator device. In some cases, a small-diameter core decompression and injection of bone stem cells into the femoral head will also be performed (these procedures are described in the “Minimally-Invasive Surgical Treatment” section of this page).
Two soft tissue releases are performed to allow the hip joint to become more mobile so that the femoral head can be placed into the proper position inside the cup before the external fixator is applied. An incision is made in the groin that is approximately 1 inch (2.5 cm) long. This incision is for the release (tenotomy) of the iliopsoas tendon. Another ¼ inch (0.64 cm) incision is made on the upper inner thigh. The inner thigh muscles are released (tenotomy) through this incision.
After the soft tissue releases are completed, the small-diameter core decompression and injection of bone stem cells might be performed. Then the arthrogram is performed to provide a record of the shape of the hip before the treatment (the arthrogram procedure is described in the “Minimally-Invasive Surgical Treatment” section of this page).
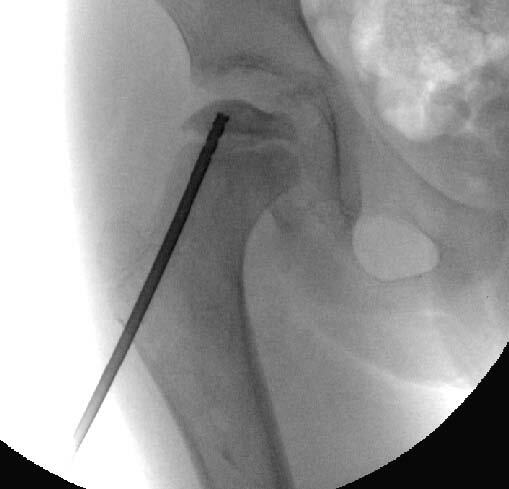
The hip is placed into full extension and approximately 20° of abduction (hip spread position) with the kneecap pointing forward. Then the external fixator is applied. This device consists of three pins above and below the hip joint. The pins are placed through the skin with very small incisions and inserted into the bone. This pin fixation allows for a very stable anchoring point for the external fixator. The external fixator contains a hinge that allows for hip flexion (sitting position) and extension (standing position). The hip joint motion is essential for cartilage healing. During the 4 months that the external fixator is in place, all other motions are restricted.
- The surgery is performed under general anesthesia and lasts 3 to 4 hours. While the child is under the effects of anesthesia, an epidural catheter is placed in the lower back. After surgery, medication is given through the epidural catheter to control pain.
- Phase 2 of Hip Distraction: Using the External Fixator to Distract and to Stretch the Hip
- Immediately after Surgery
After the external fixator is applied, the child usually stays in the hospital for 3 to 5 days. Medication is given through the epidural catheter to control pain for at least the first 2 or 3 days after surgery. This allows the child to immediately start physical therapy with minimal to mild discomfort. The child may also be given valium because it is an excellent muscle relaxant and reduces the muscle spasms, which can be as problematic as the pain. During physical therapy, the child will start range of motion exercises for the hip and knee. The child will learn to walk with either a walker or crutches with 50% weight bearing allowed on the affected hip. The physical therapist will also teach the child to transfer safely in and out of the bed, wheelchair, and toilet. We will order the child a wheelchair that reclines before the child is released from the hospital. - Distracting the Hip
 For the first two weeks after surgery (approximately), the patient and/or the family will distract the hip. The external fixator has a part called a distractor (see the labeled photo of the external fixator), which is adjusted by turning the hex screw ¼ turn twice a day (for a total of ½ mm per day). Each “turn” gently pulls the hip joint apart. When the femoral head is pulled slightly away from the cup, it is called joint distraction. Joint distraction allows the hip to be free of any force or pressure that could compress the delicate cartilage. It also encourages the cartilage to heal and grow into a more spherical shape. The child remains 50% weight bearing on the affected leg during the 4 months that the external fixator is worn.
For the first two weeks after surgery (approximately), the patient and/or the family will distract the hip. The external fixator has a part called a distractor (see the labeled photo of the external fixator), which is adjusted by turning the hex screw ¼ turn twice a day (for a total of ½ mm per day). Each “turn” gently pulls the hip joint apart. When the femoral head is pulled slightly away from the cup, it is called joint distraction. Joint distraction allows the hip to be free of any force or pressure that could compress the delicate cartilage. It also encourages the cartilage to heal and grow into a more spherical shape. The child remains 50% weight bearing on the affected leg during the 4 months that the external fixator is worn. - Stretching and Extending the Hip
The hip must be stretched and extended every day and night during the entire 4 months that the external fixator is in place. This is done by using a part of the external fixator called the extension bar (see the labeled photo of the external fixator). This adjustable and removable bar maintains full hip extension, which is essential to the treatment. When this bar is in place, the hip is locked in a straight, extended position, and no motion can occur. During the 4 months that the external fixator is applied, the bar is placed onto the fixator once or twice during the day for approximately 30 to 45 minutes. The extension bar is also placed every night and worn all night. The bar can be removed during the remaining daytime hours and during physical therapy. If the hip does not want to extend fully because it is too tight, the extension bar can be placed onto the fixator when the hip is slightly bent. Then the hip can be slowly straightened and extended by turning the adjustable nut until the hip is completely straight (fully extended). - After Being Released from the Hospital: Physical Therapy
After being released, the child will continue physical therapy 5 times per week during the distraction period (first 2 weeks after surgery). Typically, one hour of physical therapy will be in the pool, and one hour will be outside of the pool. Physical therapy is essential since the motion of the hip joint is the key to success in Perthes disease. After the distraction stage, most patients return home and attend physical therapy sessions near their home. Once the distraction has been completed, physical therapy can be reduced to 2 to 3 sessions per week if the child has good hip and knee motion. - After Being Released from the Hospital: Follow-up Appointments at the Rubin Institute
The majority of our patients at the Rubin Institute for Advanced Orthopedics come from out of town. It is helpful if patients have a primary care doctor or an orthopedic surgeon near your home for medical emergencies (which are very rare). However, if surgery is performed at our institute, we insist that the child return to our institute for follow-up appointments to ensure a successful and safe outcome. The appointment consists of conducting a physical examination, reviewing the physical therapy progress reports, and taking X-rays. A follow-up appointment is normally scheduled 2 weeks after the external fixator is applied. Usually, by this appointment, the child has already completed the distraction stage. Six weeks after the external fixator is applied, an X-ray of the hip is taken at a local doctor’s office and sent to the Rubin Institute. If the maintenance of the external fixator and the physical therapy are both going well, then X-rays will be taken every 6 weeks and sent to the Rubin Institute for evaluation until the external fixator is removed. However, if any problems occur with the external fixator or during physical therapy, then the patient and family return for an appointment. The office will talk to you about having the child measured for a Scottish Rite brace, which will need to be created and customized before the external fixator removal.
- Immediately after Surgery
- Phase 3 of Hip Distraction: External Fixator Removal
- Four months after surgery, the external fixator is removed during an outpatient surgery (meaning the child does not spend the night after surgery in the hospital) at the Rubin Institute. The removal cannot be performed by a local orthopedic surgeon. The external fixator removal surgery consists of removing the external fixator and pins, performing a hip arthrogram (explained above), injecting a Botox solution into the inner thigh muscles, and releasing tissue around each pin site to allow the pin sites to have a flattened appearance when they heal.
- Phase 4 of Hip Distraction: Wearing a Brace/Pillow, Continuing Physical Therapy and Daily Perthes Exercises, and Attending Follow-Up Appointments at the Rubin Institute
- Wearing a Brace/Pillow
After the external fixator is removed, a Scottish Rite brace or a special abduction pillow with Velcro straps is worn by the patient. The child will be able to walk and sit while wearing the brace/pillow. This brace/pillow is worn full time for 4 weeks. “Full time” means that the brace/pillow should be worn 24 hours a day unless the child is in physical therapy or exercising, swimming, bathing, or riding a bike. The brace/pillow encourages the legs to remain in semi-spread position of 20°. This is the best position for the hip during this stage of the treatment. The brace is hinged, which allows the child to bend and straighten the hip. Four weeks after the removal surgery, the child will start wearing the brace/pillow only at night and will continue to do this for the next 3 to 6 months. - Attending Physical Therapy Sessions and Continuing Daily Perthes Exercises
After the external fixator is removed, the physical therapy and home exercise program is essential. The child attends five physical therapy sessions per week immediately after the external fixator is removed. The home exercise program consists of the five stretches that make up the “Perthes exercises” (as shown in the “Non-surgical Treatment Options” section). These stretches are the true secret to success. The exercises are performed 2 to 3 times every day for the first 6 months after the external fixator is removed. Depending on the child’s progress, the physical therapy will eventually be decreased to only 2 to 3 sessions per week, but the child still needs to perform the Perthes exercises consistently 2 to 3 times every day. During the 6 weeks after the removal surgery, the child is allowed to put weight on the affected leg until he or she achieves full weight bearing. - Attending Follow-Up Appointments at the Rubin Institute
The child and family will need to return to the Rubin Institute for a follow-up appointment 6 weeks after the external fixator is removed. After that appointment, additional follow-up appointments will occur every 2 to 3 months (depending on the child’s progress) for the first year after the external fixator was applied so that we can monitor the hip.
- Wearing a Brace/Pillow
- Phase 5 of Hip Distraction: Monitor and Maintain Progress
- Our goal is that 6 to 8 months after the external fixator is applied, the child will no longer use the brace/pillow at night and will be able to participate in all physical activities. The Perthes exercises need to be performed daily, but they need to be done only once a day. Most patients ask how long they will be required to continue the Perthes exercises. Our center recommends that the Perthes exercises continue until the child graduates from high school. The patients who have excellent outcomes, (even if the shape of the femoral head is not ideal), are the patients with excellent hip motion. In Perthes disease, hip motion equals success. Success means that the child is not in pain and can return to all previous activities.
When more than a year has passed since the external fixator was applied, the number of office appointments per year at the Rubin Institute decreases to only one appointment every 6 to 12 months until the child is approximately 18 years old. These appointments allow our doctors to monitor the hip growth and hip range of motion. The appointments are also an opportunity to remind the child about the importance of the Perthes exercises and to assess the final shape of the femoral head at the end of growth.
- Our goal is that 6 to 8 months after the external fixator is applied, the child will no longer use the brace/pillow at night and will be able to participate in all physical activities. The Perthes exercises need to be performed daily, but they need to be done only once a day. Most patients ask how long they will be required to continue the Perthes exercises. Our center recommends that the Perthes exercises continue until the child graduates from high school. The patients who have excellent outcomes, (even if the shape of the femoral head is not ideal), are the patients with excellent hip motion. In Perthes disease, hip motion equals success. Success means that the child is not in pain and can return to all previous activities.
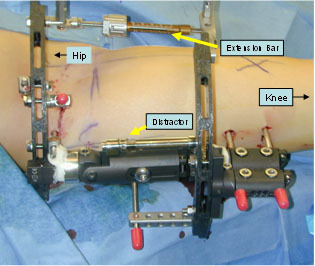
Example of Hip Distraction Treatment
 Eleven-year-old boy with late-onset Perthes disease. He previously underwent a shelf procedure at another institution that failed.
Eleven-year-old boy with late-onset Perthes disease. He previously underwent a shelf procedure at another institution that failed. X-ray shows the hip during hip distraction. Note that the femoral head is completely contained inside the hip cup.
X-ray shows the hip during hip distraction. Note that the femoral head is completely contained inside the hip cup.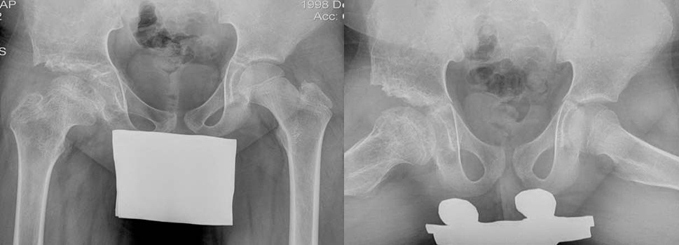 These X-rays show the hip one year after hip distraction treatment. The hip has full range of motion, and the boy is not in pain.
These X-rays show the hip one year after hip distraction treatment. The hip has full range of motion, and the boy is not in pain.What are some of the logistical issues for children undergoing hip distraction treatment?
Most patients who undergo treatment are not from Baltimore, Maryland. There are three main strategic approaches to the logistics behind undergoing hip distraction treatment:
- Strongly recommended option: The family and patient come for the surgery and plan to stay in town for an additional 2 weeks after being released from the hospital. The child attends physical therapy at Sinai Hospital for these two weeks. This strategy has multiple advantages. First, our therapists have the most experience with the external fixator and the hip distraction treatment. This therapist will be able to educate the child and family so they understand what adequate therapy should look like. The family can also record a video of the therapy so that they can show it to their physical therapist at home. This will be extremely important when the child transitions to a local physical therapist. Our physical therapists can communicate directly with the patient’s local physical therapist and explain our protocol.
Second, the therapy is performed on-site at the Rubin Institute. If there is a medical concern or question, the family simply comes upstairs and can be evaluated by the physician or physician assistant in a timely manner. It is important to have access to our physicians and our physician assistants immediately after the child is released from the hospital with the external fixator. Most parents have many questions as to what is normal or what is to be expected. Staying in the area for the first week or two after release from the hospital will give families time to adjust to life with an external fixator and will allow us to closely monitor the treatment. Families will also be in town for the first follow-up appointment two weeks after surgery. After the patient returns home, the X-ray evaluation and clinic visits remain the same as stated above.
- The family and child come for the surgery. The child stays in the hospital for 3 to 5 days. After being released from the hospital, the family returns home, and the child begins physical therapy with a local therapist. The family and patient come to the Rubin Institute for all required follow-up appointments, external fixator removal surgery, etc.
- The final strategy is for the patient and family to stay during the entire external fixator treatment time (4 to 5 months). This is usually reserved for families in special circumstances or who are from other countries.
For information on convenient and affordable housing for your stay, please see our Plan Your Trip to Baltimore section of the website.
Why choose the International Center for Limb Lengthening for treatment of Perthes disease?
Treating Perthes disease is a complex process. Our doctors will take the time to make sure you understand all of the options and then will customize your child’s treatment to meet his or her specific needs. Our patients also benefit from our team-centered approach with world-renowned pediatric orthopedic surgeons, anesthesiologists with extensive experience working with pediatric patients, and specialized physician assistants, nurses, and physical therapists. We also have a large group of patient families who have children undergoing Perthes treatment that offer support through our International Center for Limb Lengthening (ICLL) Facebook Group, ICLL Families. We help patients with Perthes disease achieve their best possible result.
Handouts
- “Perthes Perspective: An Approach to Treatment”
- “Perthes Disease: Timeline for Hip Distraction Treatment”
- “Perthes Stretching Exercises”
- “Three X-ray Views of the Pelvis”
Videos
Chat with a doctor about Perthes disease
Our doctors hold free monthly chats on various subjects, including Perthes disease. Click here for more information about our monthly chats.