Posteromedial Tibial Bowing (PMTB)
 Ally with even legs after successful PMTB treatment. For more of Ally’s story, click here.
Ally with even legs after successful PMTB treatment. For more of Ally’s story, click here.What is posteromedial tibial bowing (PMTB)?
Posteromedial Tibial Bowing (PMTB), also sometimes called congenital posteromedial bowing of the tibia (shin bone), is an uncommon condition. When a baby is born with this condition, the foot is bent up on itself to the point where the top of the foot is almost touching the front of the shin bone.
Some advocate that this deformity is due to a packaging problem in the intrauterine environment or secondary to rupture of the amnion–the innermost membrane that encloses the embryo. However, this condition represents a true underlying bone growth deformity or dysplasia. This is evident by the size difference of the feet and the leg length difference that develops over time.
This deformity consists of an actual bend in the middle of the tibia, an inward twist of the tibia and an outward deformity of the ankle joint. Amazingly, this deformity can resolve spontaneously over the first two years of growth. Unfortunately, the spontaneous resolution does not always occur. Most doctors will continue watching a child with significant deformity waiting for it to resolve while secondary deformities at the knee and ankle develop. The vast majority of the original deformity should be resolved by the second year of life. If significant angular deformity persists after the age of 18 months, or a persistent severe inward twist of the lower leg is present, then a more aggressive treatment strategy is needed. Also, if secondary deformities develop at the knee or ankle level, more aggressive treatment should be started.
Children with posteromedial tibial bowing also develop a leg length discrepancy on the affected leg. The amount of the leg length difference can be 4 to 10 cm (1.6 to 4 inches) by the end of growth (14 years for girls and 16 years for boys). The amount of the final limb length discrepancy can be predicted using the Multiplier App developed at the International Center for Limb Lengthening of the Rubin Institute for Advanced Orthopedics.
Sometimes the ankle and subtalar joints can be negatively affected, because they twist into a configuration that compensates for the bowed deformity in the shin bone. If left untreated, the shin bone will mostly correct itself, but the resulting ankle and subtalar deformity may become rigid due to tightening of the muscles, called a contracture, around the ankle joint.
How is posteromedial tibial bowing treated?
The goal of treatment in posteromedial tibial bowing is for the child, when fully mature, to have straight legs of equal length. Treatment must be individualized for each child, taking into account the predicted height and the predicted limb length discrepancy. Both of these can be estimated with the Multiplier App.
During infancy, we recommend splints and stretching exercises to help speed up the correction of the soft tissue contractures and encourage the remodeling of the severe angulation. Once the infant becomes a toddler and significant spontaneous correction of the deformity has occurred, we often prescribe shoe modifications to keep the hindfoot aligned with the rest of the lower half of the shin bone. These shoe modifications are essentially a shoe lift that also includes a “shim” to account for the angulation and the limb length discrepancy.
The child is followed every six months with clinical and radiographic (X-ray) examination to document the remodeling of the deformity. If the original deformity resolves, then only the leg length discrepancy needs to be managed and eventually corrected.
If the original deformity has not resolved by 14-16 months of age, then an earlier definitive correction is recommended with surgery. The surgery includes cutting of the tibia and fibula bones (osteotomies) at the level of the angulation or deformity. An external fixation device is used to to gradually lengthen the bone and correct the angular deformity. The lengthening adjustments are very small–less than a millimeter (0.04 in)–and they do not cause significant pain. There can be a sensation of tightness or ache towards the end of adjustments, but this is managed with therapy and medication. The lengthening rate is usually 1 cm (0.4 in) of length for every two weeks of external frame adjustments.
Once the lengthened bone is well-healed, the external fixator is removed and a cast is put on for one month. At the time the external fixator is removed, an internal wire or plate can be inserted to protect the newly healed bone. The posteromedial bowing does demonstrate a slower healing rate than “normal” bone. This is more evidence that this is a true bone dysplasia and not just a position or packing disorder. After cast removal, the patient continues recovery with physical therapy and increased activity level. Usually a short leg brace is used for one to three months after correction. This early and more definitive treatment protocol allows for more normal ankle growth and development as compared to patients treated later in childhood or pre-adolescence.
A second lengthening may be necessary when the child is a teenager if there will be a significant limb length discrepancy. For some children, these lengthening treatments can be paired with stunting the growth of the longer limb around ages 10-12 years in an effort to minimize the amount of lengthening needed. This minimally invasive procedure is called epiphysiodesis. If the overall predicted leg length discrepancy at the end of growth is less than 5 cm (2 in), then only a slowing of the growth (epiphysiodesis) on the lower leg might be required to achieve equal leg lengths. The decision to perform lengthening versus shortening is a decision for the parents and patient. The only side effect of shortening is the loss of final height by the amount the long leg is shortened.
Older children who were not treated as toddlers can undergo more complex surgery to correct the persistent deformity, the secondary deformities and the leg length discrepancy. This usually requires a double level or two bone cuts (osteotomies) in the tibia to straighten the deformity. Either at the same time of the osteotomies and application of the external fixator, or in a future procedure, the hidden ankle deformity is also addressed with a minor guided growth screw. The rate of lengthening while using the external fixator is usually the same for this age group with 1 cm (.04 in) of length gained every two weeks.
For adolescents presenting with residual deformity and leg length discrepancy secondary to posteromedial bowing of the tibia, the treatment is similar to that of the older children discussed above. The tibial deformity is corrected with a double osteotomy (two bone cuts) and placement of an external fixation device. Since the adolescent patients have either completed their leg growth or are close to the end of leg growth, the definitive lengthening and equalization of the leg can be performed at the same time as the deformity correction.
The posteromedial bowing deformity can be corrected at any age; however, there are significant advantages of correcting the original deformity at a younger age. As stated earlier, if a persistent deformity is still present at the age of 18-24 months then a corrective osteotomy should be performed. This allows the lower extremity to grow and develop in a more “normal” fashion, which decreases the secondary deformities that could permanently alter the function of the knee, foot and ankle.
What is a typical posteromedial tibial bowing treatment timeline?
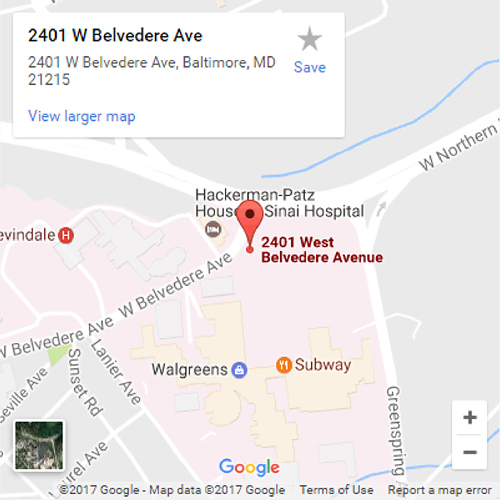
Most patients need to be in Baltimore for between 4-8 weeks for the surgery and initiation of physical therapy. The typical treatment timeline is as follows:
- The patient comes to clinic for a preoperative visit the Monday before surgery.
- Surgery usually occurs on a Tuesday or Wednesday.
- The patient will stay in the hospital for 2-4 days post-surgery.
- After surgery, the bones are allowed to rest for 5-10 days to begin the healing process; this period of time is called the latency period. The bone resting time varied depending on the age of the patient, the bone-cutting technique and the underlying diagnosis that is being treated.
- The patient comes to clinic for the first post-operative visit the Monday after surgery. Follow-up clinic visits will be scheduled every two weeks until lengthening ends. Lengthening usually ends after the 10-12 week mark, depending on the amount of length being achieved. The rule of thumb is that for every 1 cm (0.4 in) of length, it takes 2 weeks of external fixation lengthening adjustments.
- Lengthening begins after the first postoperative visit (usually between 5-10 days after surgery—after the latency period). The patient family will participate in an educational session to learn about the external fixator and how to adjust and care for it. Physical therapy usually starts the same day as the postoperative visit and will occur Monday-Friday for 1-2 hours per day. This can consist of land and water therapy. The patient will be allowed to fully weight bear as soon as s/he is comfortable enough to do so.
- It is crucial that the initial physical therapy be performed in Baltimore with our staff of specialized physical therapists. This therapy can be transferred closer to home within the first 4-8 weeks. However, the patient still needs to be seen in our clinic for close follow-up every two weeks until the external fixation adjustments are completed.
- After the last external fixator adjustment has been completed, and the final office visit determines that the goal of bone length and position has been achieved, the patient can return home if s/he is not from the Baltimore area or has yet to return home. The patient will need to have X-rays taken and sent to the surgeon every 4-6 weeks until the bone has fully healed. The external fixation device stays in place until full healing has been achieved. The external fixator acts as the deformity corrector during the first phase of treatment that is called the distraction phase. Then the external fixator acts as a bone stabilizer during the second phase of treatment called the consolidation or healing phase.
- The consolidation or healing phase can last 2-4 months depending on the rate of bone healing. During this period, the patient will continue physical therapy 2-3 times a week.
- Once the X-rays demonstrate the bone has fully healed, the patient will need to return to the International Center for Limb Lengthening in Baltimore to have the external fixation device removed.
- The external fixator removal is usually an outpatient surgery. During this surgery, the external fixation device is removed and a long leg cast is placed. Afterwards, patients not from the Baltimore area can return home. The long leg cast remains in place for 4-6 weeks. The patient will be allowed full weight bearing in the cast.
- 4-6 weeks after cast placement, the patient will need to return to the International Center for Limb Lengthening for final cast removal and X-rays. During this visit, physical therapy instructions will be given along with any activity modifications. For patients not from the Baltimore area, they can return home and the next several follow ups can be made via email and X-rays sent from home or by telemedicine.
- If all has gone according to plan, the patient will then return to Baltimore for annual checkups.
What complications can occur during the treatment process?
The most common complications are pin-site infections, loss of knee motion and slow bone healing.
- Pin-site infections are not uncommon during an external fixation treatment. This type of infection most commonly represents a simple superficial skin infection that presents with increasing pain at the site. Other signs might be pain with redness or drainage. Our staff will teach the patient and/or family more details about these symptoms and proper pin-site care before the patient leaves the hospital. Adequate pin-site care is the best way to avoid pin-site infections. For more information about pin-site infections, please see this page.
- Loss of knee motion can occur during the lengthening period. If this happens, then accurate X-rays are very hard to obtain. Contractures also make walking difficult and lead to more discomfort. The way to avoid this problem is the daily physical therapy during the lengthening period followed by physical therapy 2-3 times per week during the healing phase. Also, a removable brace will be made to keep the knee straight at night. The brace will be provided either during the hospital stay or at the first postoperative visit.
- Slow bone healing can occur due to the underlying pathology of the posterior medial bow. We do not know why this happens. The way to avoid this problem is to carefully adjust the rate of distraction (slow down or speed up the lengthening rate) according the bone appearance on the X-rays that are taken every two weeks. Also, proper nutrition is very important; Vitamin D, Vitamin C, calcium and protein are essential. For more information, see our page Encouraging Bone Healing.
- If the bone heals poorly–either incompletely or with a thinner bone segment–this might require an insertion of a simple wire from the bottom of the foot and up the tibia to stabilize the bone from the inside. This is termed prophylactic fixation of the tibia. This wire remains in place during the initial 4-6 weeks of casting after the external fixator is removed. The only difference at the time of the cast removal is that the wire is also removed. To remove the wire, a brief outpatient anesthetic/sedation is needed in the operating room instead of a clinic visit. If the bone healing is significantly deficient, then a prophylactic plate insertion is required. This would necessitate an overnight stay instead of an outpatient visit at the time that the external fixator is removed. These surgical strategies for poor healing can be determined prior to the external fixator removal so the family can plan accordingly.
Why choose the International Center for Limb Lengthening for treatment of posteromedial bowing of the tibia?
Limb Lengthening and deformity correction are complex processes. Our pediatric orthopedic team has over fifty years of combined experience in limb lengthening and reconstruction and extensive experience treating this specific condition. Your doctor at the International Center for Limb Lengthening (ICLL) will take the time to make sure you understand all of your options and then will customize your treatment to meet your specific needs.
An apartment-style housing facility, the Hackerman-Patz House, was built across the street from the hospital to accommodate families during treatment. The Baltimore Ronald McDonald House also is available for families to stay at while a child undergoes treatment, and it provides a shuttle service to the ICLL. Our patients find both housing options provide a supportive family atmosphere.
Our patients benefit from our team-centered approach with world-renowned surgeons and specialized physician assistants, nurses and physical therapists. We help patients with posteromedial bowing of the tibia achieve their best possible result.
Chat with a doctor about posteromedial tibial bowing
Our doctors hold free monthly chats on various subjects, including posteromedial tibial bowing. Click here for more information about our monthly chats.