Bone Grafting
What is bone grafting?
Bone grafting is a procedure where damaged bones can be repaired or rebuilt using transplanted bone from another source. Sources for transplant bone include the patient (autograft), a cadaver (allograft) or synthetic bone.
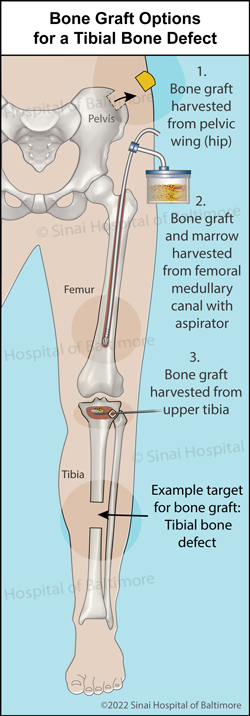
An autograft takes bone from another area of the patient’s body (donor bone), and moves it to the broken bone that needs extra support (graft). This bone comes from an area that will not cause problems upon removal. A common area to harvest the donor bone from is the pelvic wing (hip). This bone contains the patient’s own live bone cells, which can help stimulate healing in a different part of the body where healing is defective. It also acts as a scaffolding for new bone to grow into.
Allograft bone comes from a cadaver. This is usually obtained through a bone bank, similar to a blood bank. Like any organ, bone can be donated after death, and kept in a bank for future use. Unlike an autograft, the allograft does not contain live cells, and purely acts as a structural scaffold for the patient’s bone to grow into. The patient’s bone will eventually replace the donor bone as more growth occurs. There is minimal risk of disease transmission from the donor to the patient, as the bone graft is typically sterilized.
Synthetic bone is composed of calcium and commonly called a “bioceramic.” It is similar to autograft bone in shape and consistency. Bioceramics also have the advantage of being available in large quantities.
Another option some surgeons use is bone morphogenic protein (BMP). This is a group of growth factors in the body that promote bone growth, and when concentrated, can be useful in helping the patient’s bone to heal. It has very powerful bone-forming abilities, and must be used safely as determined by your surgeon. BMP is produced in the lab, so there is no risk of disease transmission.
When is bone grafting a good option?
Bone grafts are a good option for patients who have damaged or diseased bone and require extra support to repair it. It is commonly used when patients have fractures that have not healed well, or to fill defects caused by trauma (injury), infection, and/or disease. In some cases, the broken bones are in good contact, but there is a lack of healing. Bone grafting stimulates healing in such situations. In other cases, there is a structural defect or gap. Bone grafting fills thin defects, and allows healing.
What happens during the bone grafting procedure? Each procedure can vary according to the needs of the patient, and should be discussed with your surgeon prior to any operation. Most patients will receive anesthesia before surgery so there will not be pain or discomfort during the procedure. The affected area, (e.g., leg), and the donor area, (e.g., hip), will be cleaned and prepared for surgery. The surgeon will harvest the bone graft from the donor site. The healthy donor graft will be transferred to the bone needing support, typically as morselized bits. Additional required procedures to stabilize the bone may be completed as well. There may be some pain for a few weeks at the donor (harvest) site.
How long does a bone graft procedure last?
The procedure length depends on the complexity of the case and the size of the bone that must be either harvested or fixed. Most bone graft surgeries last between 1-2 hours.
How long must patients stay in the hospital after the bone graft procedure?
Depending on the patient and the extent of the surgery, it is possible to go home the same day as the surgery. Patients will receive instruction on proper activity after the surgery and on how to care for the treated area, including activities and movements to avoid. Depending on the specific case, you may also need to wear a cast or brace while the bone graft heals.
What are the benefits and risks of bone grafting?
The anticipated benefits of a bone graft include successful repair of a broken bone, strengthening of a weak bone, and providing a framework for better patient bone growth and maintenance of bone structure. The risks of bone graft surgery include: pain, swelling, infection, blood clots, nerve injury, bone graft rejection, inflammation and reabsorption of the graft.
On the surface it may appear that allograft (bone graft removed from a cadaver) and synthetic graft (made in a laboratory) have the advantage of avoiding the risks and pain associated with harvesting graft from a donor site in your own body. However, the “gold standard,” highest quality and most effective bone graft material is still from your own body. Therefore, for most, but not all situations, auto-graft is used.