Ulnarization
For a printable handout on ulnarization treatment for club hand, please click here.
What is ulnarization?
Ulnarization is a surgery used to treat radial club hand, (also known as radial dysplasia or radial aplasia), by correcting the deformity and achieving normal alignment of the wrist. In this surgery, the hand and carpus (wrist bones) are moved to the ulnar side (little finger side) of the ulna (one of the two long bones in the forearm, on the side opposite to where the thumb would normally be). The deforming forces around the hand and wrist are converted to stabilizing forces by using the distal ulna (weight-bearing part of the wrist joint) as a fulcrum (balancing point). Although some institutions use other procedures such as radialization and centralization, our center has had better results using ulnarization, with no recurrence of the deformity since we started performing the procedure in 2003. In this surgery, an external fixator is used post-operatively to maintain the corrected position for three months.
At what age is ulnarization surgery performed?
Ulnarization is typically performed between twelve to eighteen months of age, but can be done on children as old as ages six to eight years. Families can have an initial evaluation for younger children whenever it is convenient for them. Many families feel more comfortable having an earlier evaluation so they can better understand the process and start planning ahead.
What happens at the initial evaluation and pre-surgical appointment?
New patient evaluations take several hours. When the patient returns in the future for surgery, they will also generally need a pre-surgical appointment to review the plans, get final X-rays and photographs and sign consent forms. If the family is coming from a great distance, for example from overseas, these can usually be done in one trip. Note that some insurance companies may need more time between the evaluation and the surgery authorization.
What are other common surgical treatment options for radial dysplasia?
The most common surgical treatment options for radial dysplasia are centralization and radialization. Both of these procedures attempt to place the hand and carpus (wrist bones) on the end of the ulna. The diagram below demonstrates the positioning of the hand/carpus after centralization, radialization and ulnarization. Both centralization and radialization are limited by high recurrence rates of deformity, growth arrest of the distal ulna physis (growth plate) and loss of wrist motion.
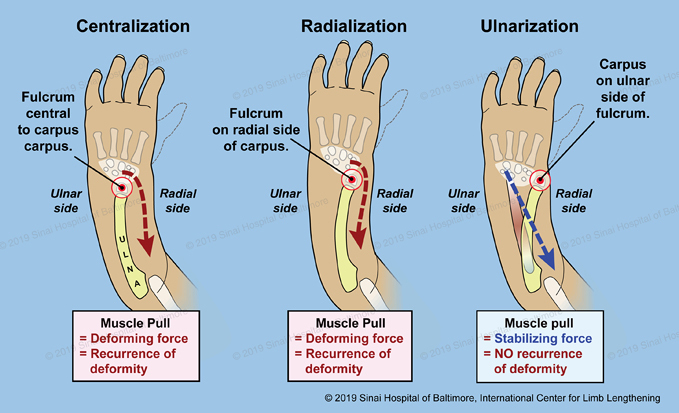
The centralization procedure attempts to balance the hand and wrist on a rounded end of the ulna. The tight tissues create a deforming force that eventually pulls the hand back into a radial club hand position. If the correction is maintained, this usually means the carpus (wrist bones) have fused to the end of the ulna with permanent loss of wrist motion and loss of ulna growth potential.
The X-ray below shows a 19-year-old female who had a centralization procedure at the age of 18 months. The wrist is fused and the ulna is only 8.5 cm (3 1/2 in) in length.

The radialization procedure was developed to attempt to decrease the recurrence rate of the radial club hand deformity after centralization. The radialization includes a hand and carpus position farther to the ulna (little finger) side of the distal ulna and a transfer of the radial based muscles to the ulnar-based muscles. The muscle transfer is an attempt to balance the deforming forces around the hand and wrist. Unfortunately, these muscles that are used in the radialization are rarely present in the severe forms of radial dysplasia. If these muscles are present, they are very small and weak. Similar to the centralization procedure, the radialization procedure has a very high incidence of recurrent club hand deformity, distal ulna growth arrest and stiffness of the wrist.
The diagram above also demonstrates a schematic of the ulnarization procedure where the hand and carpus are moved to the little finger side of the ulna. The deforming forces are now converted to stabilizing forces by using the distal ulna as a fulcrum. The ulnarization procedure has the advantages of maintaining wrist motion and distal ulna growth. Our center has not experienced a recurrence of radial club hand deformity since using the ulnarization technique in 2003.
What is the ulnarization strategy for radial dysplasia?
As described above, the ulnarization procedure was developed as a modified approach to radial dysplasia by Dr. Dror Paley. The concept was to perform a comprehensive release of the radial club hand deformity through an extensive exposure of the volar (palm side) of the wrist and forearm. The wrist/carpal joint capsule is released and the hand and carpus is transferred to the ulna side of the ulna. As demonstrated in the diagram above, the deforming forces causing the radial club hand deformity are now converted into stabilizing forces using the distal ulna as a fulcrum.
This position is held with an external fixation device postoperatively for three months to allow fibrous healing and stabilization of the new hand position. This essentially creates a syndesmosis or fibrous joint connection between the carpus (wrist bones) and the distal ulna. This is similar to the joint between the distal tibia and fibula just above the ankle joint. The advantage of a syndesmosis type joint formation in the wrist is maintained wrist motion along with stability of hand position.
The previous radial club hand correction techniques, both centralization and radialization, create either a synchondrosis (cartilage to cartilage connection) or synostosis (bone to bone connection) resulting in the loss of the wrist joint and wrist motion. Another technical difference in the ulnarization technique is the transfer of the Flexor Carpi Ulnaris muscle (FCU) to the back of the hand to increase wrist extension (pulling the hand up) power. The centralization and radialization techniques describe transferring muscles on the radial side of the forearm; however, these muscles are rarely present.
In contrast, the ulnarization technique utilizes the flexor muscle on the ulna side of the forearm that is always present and very strong. This muscle is detached from its connection on the palm side of the wrist, where it acts more as a deforming force, and is transferred or moved to the back of the wrist to improve wrist position and motion. Enhancing wrist extension is important due to the fact that the most functional hand position is neutral position to 15-30 degrees of wrist extension.
What is the ulnarization technique?
The following is a schematic explanation of the ulnarization procedure:
- An incision is performed on the palm (volar) side of the hand and forearm in a zig-zag fashion. This style of incision helps to increase exposure and to avoid crossing the wrist flexion creases with a perpendicular incision. Crossing skin creases in a perpendicular incision increases the risk of scar contractures of the adjacent joint, so this is avoided.
- After the skin flaps are carefully elevated, all vital structures are identified. The ulna nerve and ulna artery are isolated and protected. The Flexor Carpi Ulnaris muscle (FCU) is identified and traced to its connection to the pissiform bone (part of the carpus).
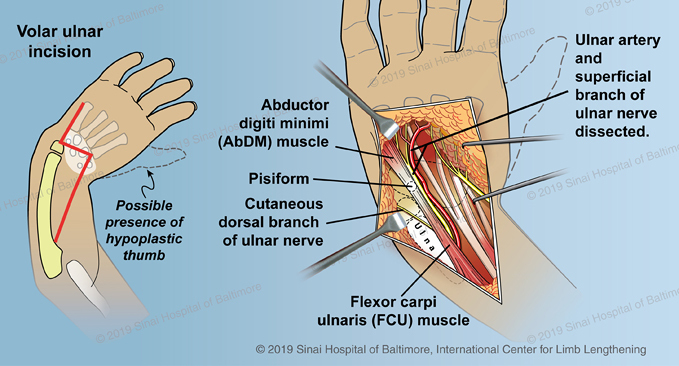
- A portion of the pissiform bone along with the FCU muscle is released from the remainder of the carpus and elevated in preparation for transfer later in the procedure.
- The central and radial zones of the wrist are explored to identify all flexor tendons, the median nerve and any fibrous radial remnant. The “radial pocket” is created to allow room for the eventual transfer of the distal ulna.
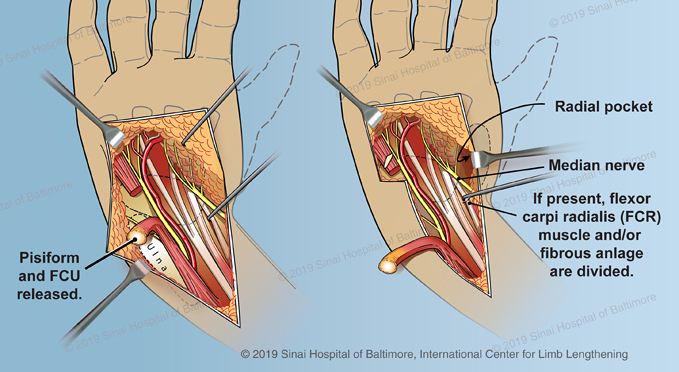
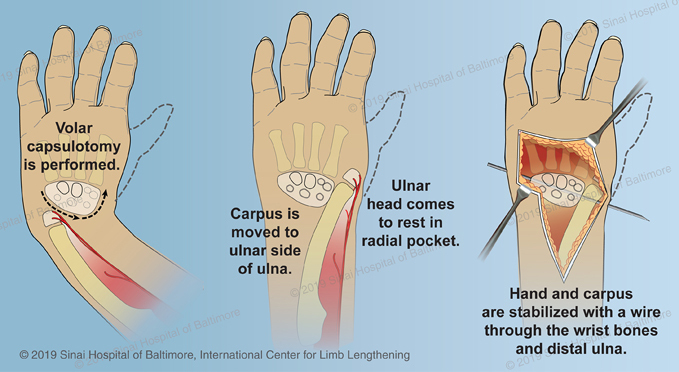
- After all the important structures are identified and protected, the fibrous capsule around the wrist bones (carpus) is released. This is termed the volar capsulotomy.
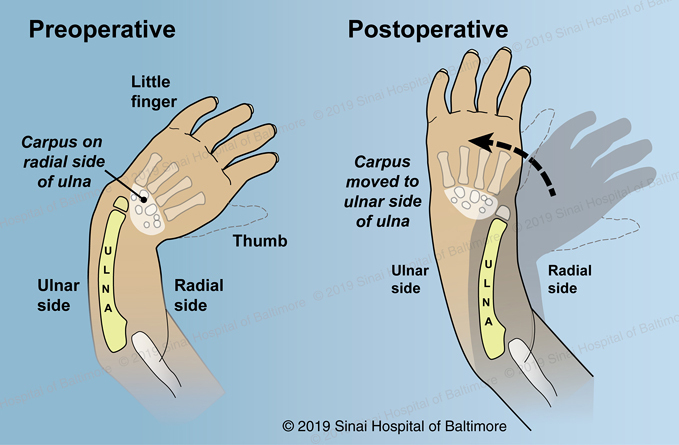
- Once the carpus is mobile and freed from the distal ulna, the hand and carpus are moved or transposed to the opposite side of the ulna. The hand and carpus are now located on the “ulna” side of the ulna, thus the procedure’s name, ulnarization.
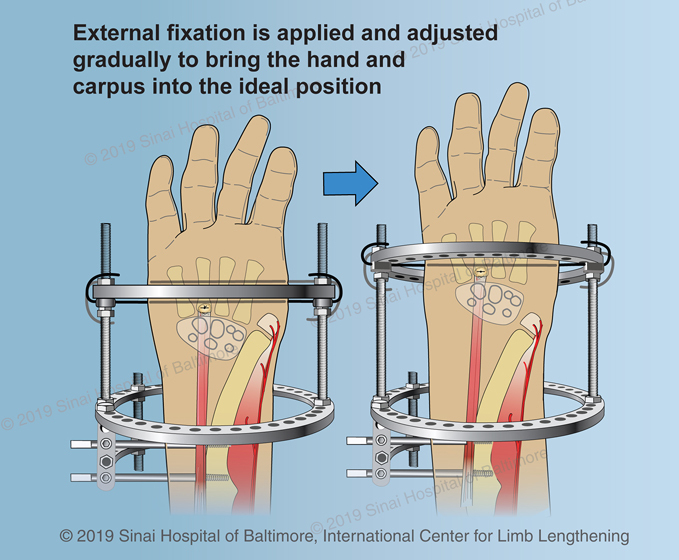
- The hand and carpus are stabilized with a wire through the wrist bones and distal ulna. If the desired position of the carpus in relation to the distal ulna is achieved at the time of surgery, the wire is left in place and an external fixation is placed to hold the reconstruction stable. This type of external fixation device will not need adjustments or turns.
- The correct position of the wrist bones or carpus is next to the distal portion of the ulna. The most distal part of the ulna is still cartilage in most toddlers and does not appear on X-rays. It is not uncommon for the hand and wrist to “settle” more distal to the correct position at the time of surgery. If this occurs during surgery, then the initial stabilizing wire that is inserted between the carpus and distal ulna is removed after the external fixation device is applied. The external fixation is adjusted gradually during the first two weeks after surgery to slowly distract or pull the hand and carpus into the ideal position. After the ideal hand and carpus position is achieved and confirmed with X-rays, the external fixation device is maintained for a total of 3 months.
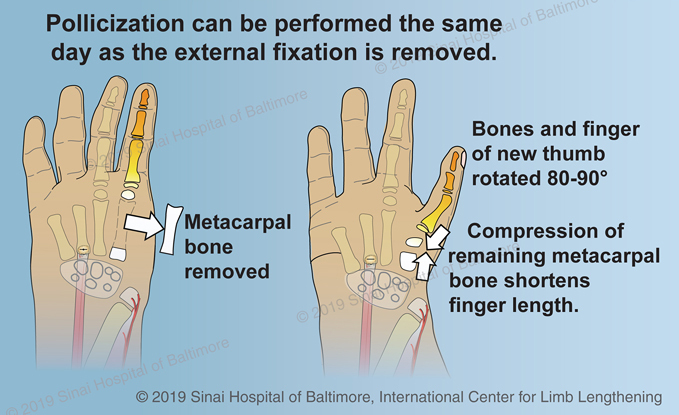
- If a pollicization (creating a functional thumb by transferring another finger to the thumb position) is needed, this can usually be done at the time of the removal of the fixator.
A case example of intra-operative photos before and after ulnarization prior to application of the external fixation device is below.
The following is a case example of intra-operative photos before ulnarization, after ulnarization and external fixation, after external fixation removal at three months, and after pollicization was performed the same day as the external fixation removal.
 Before ulnarization
Before ulnarization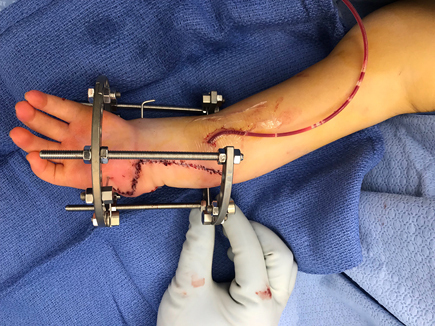 After ulnarization and external fixation
After ulnarization and external fixation
 External Fixator Removal at 3 months
External Fixator Removal at 3 months Pollicization performed same day as external fixator removal
Pollicization performed same day as external fixator removal
When does surgery take place, and how long is the hospital stay?
Surgery usually takes place on a Tuesday or Wednesday. The patient stays in the hospital approximately one to two days.
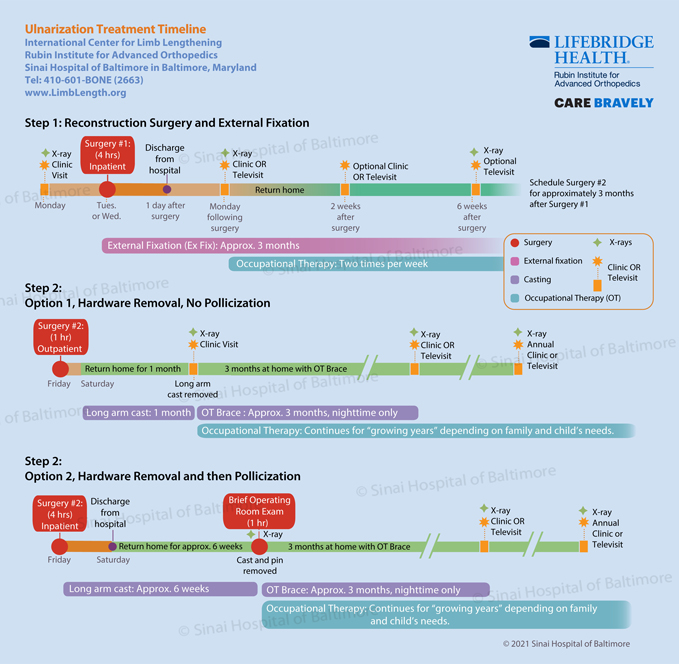 Click here for a helpful ulnarization treatment timeline.
Click here for a helpful ulnarization treatment timeline.How long does the patient need to stay in Baltimore post-surgery, and what occupational therapy is necessary?
We recommend that the patient stays in Baltimore for at least 2 weeks after the surgery, however some international patients choose to stay until the external fixator is removed to reduce travel costs. Depending on how the child is doing, some families may be able to return home sooner. The patient needs occupational therapy two times per week during the time that the fixator is on. Patients are responsible for paying for housing while they stay in Baltimore and we can direct you towards various priced options including the hospital’s Hackerman-Patz House and the Ronald McDonald House.
When is the external fixator removed?
The fixator is removed after approximately three months, and we prefer that this take place in Baltimore, since other surgeons who are not familiar with the ulnarization procedure may not understand what has been done and how to interpret any X-rays. This removal surgery is done in the operating room.
If a pollicization is needed, when and where is it performed?
If your child needs a pollicization, (creating a functional thumb by transferring another finger to the thumb position), this can usually be done at the time of the removal of the fixator. Pollicization is a much more common procedure than the ulnarization, so for financial reasons some international families choose to have that procedure done at home if it is covered by their health plan. It is important to find an experienced surgeon for the pollicization procedure.
What happens after the removal of the external fixator?
After the external fixator is removed, if a pollicization was not performed, the patient is placed in a cast which stays on for approximately 4 weeks. The cast removal is not a surgery; it is done in the clinic area. In some cases the physician may allow the cast to be removed by the patient’s home surgeon. An occupational therapist makes a custom resting splint for the child at a follow-up appointment in the clinic. This resting splint is only worn at night until the child outgrows the splint (anywhere between one and six months).
However, if a pollicization was performed, then the cast will need to stay on for approximately six weeks. The cast will need to be removed in the operating room at Sinai Hospital for detailed evaluation of the new thumb and removal of pins that are used in the pollicization procedure. After the cast is removed, an occupational therapist will make a custom resting splint for the child. It is worn day and night for one month, and then only at night until the child grows out of it, (anywhere between one and six months).
Why choose the International Center for Limb Lengthening for ulnarization surgery?
Our center has not had a recurrence of radial club hand deformity since we began using the ulnarization surgical technique in 2003. There also is no growth arrest of the ulna, so this bone can continue to grow for many years as the child grows. The child’s resulting hand is in a much more functional position with improved grip strength and wrist mobility.
Our patients also benefit from our team-centered approach with world-renowned pediatric orthopedic surgeons, anesthesiologists with extensive experience working with pediatric patients, and specialized physician assistants, nurses and physical therapists. We also have a group of patient families who have children undergoing radial club hand treatment that offer support through our International Center for Limb Lengthening (ICLL) Facebook Group, ICLL Families. We help patients with radial club hand achieve their best possible result.